Breast cancer: tools for early diagnosis
Breast cancer is the most frequent neoplasm in women and it has been shown that about one in eight women will develop it during their lifetime. Early diagnosis is possible
Risk factors for breast cancer
Let’s start with risk factors. They are different and affect women in different ways.
For example, age, as the incidence increases with age: early menarche or late menopause widens the oestrogen window, while pregnancy and breastfeeding are protective.
There is also heredity of some forms of breast cancer, which is linked to genomic alterations (the best known are BRCA1 and 2) and a certain familiarity that determines a greater predisposition to the development of this neoplasm.
Lifestyle habits (which we can always improve) are also a risk factor: obesity, which leads to altered hormone production, is a risk factor, as are smoking and alcohol; while physical activity is protective and should always be encouraged.
A further role is played by hormone therapies: in particular hormone replacement therapy in the post-menopausal period and hormone therapies for the treatment of infertility require targeted follow-up programmes for the possible early detection of carcinoma.
Symptoms of breast cancer and the importance of self-examination
Unfortunately, in the majority of cases, breast cancer does not have painful symptoms; the most common sign is a lump of hard, non-mobile, new-onset consistency; sometimes the overlying skin may be reddened and retracting with evidence of pores, and identifiable as ‘orange peel skin’.
Other associated signs may be nipple retraction (‘it was never like this’) and bleeding.
Knowledge of self-examination manoeuvres is therefore of paramount importance: these should be performed as early as 20 years of age, once a month and a week after the menstrual cycle.
A visual check is also good: in front of a mirror to observe any new asymmetries or structural alterations.
If any of the above-mentioned alterations are found, it is important to visit your doctor, who will refer you for a breast examination.
Mammography
Mammography is the pivotal investigation in screening and early diagnosis of breast cancer, as it makes it possible to highlight the signs of a possible neoplasm before it becomes clinically manifest.
It is a non-invasive test that uses low-dose ionising radiation and is performed in two projections with compression of the gland itself by the mammographer, which may cause discomfort, but hardly any real pain.
Since ionising radiation (albeit at low doses) is involved, it is important to inform the technician carrying out the test of the date of the last mammogram so as not to perform more than one a year, unless it is deemed necessary for in-depth diagnostics.
It is also not recommended to perform mammography before the age of 40, both because of the young age and because the breast would be too dense to show small lesions.
This test cannot be performed by pregnant women unless strictly necessary and on doctor’s prescription, while there are no contraindications during breast-feeding or for those with breast implants.
It is also preferable to undergo the test within the first 7-10 days of the cycle, while it would be better to avoid the premenstrual phase as it would be more uncomfortable.
It is important to bring old mammograms that have been taken (not just the most recent one) on the day of the test, so that comparisons can be made and new changes in the glandular parenchyma can be more easily detected.
This investigation allows the visualisation of parenchymal distortions or the appearance of suspicious micro-calcifications with a sensitivity that varies depending on the glandular density of the breast being tested: in fact, it will be easier to assess a more adipose breast than a very dense breast where small parenchymal distortions may be masked by the breast parenchyma. In the latter case, an ultrasound investigation is also indicated.
If any abnormality is found or there is a diagnostic doubt, the patient is referred for further diagnostic investigations, such as ultrasound (if not already performed), tomosynthesis, targeted enlargement or possibly even a level III investigation such as MRI.
Tomosynthesis is a three-dimensional high-definition mammography that allows the study of the breast parenchyma ‘in layers’ so as to allow a more detailed study of parenchymal distortions, even in dense breasts, and increase diagnostic accuracy.
Targeted mammographic enlargement, on the other hand, is performed with special lenses that focus the investigation on the glandular portion where the diagnostic doubt lies; it is especially useful in the case of suspected micro-calcifications, to assess their distribution and morphology, but also to more accurately assess parenchymal distortions and ensure that they are not a mere artefact on the mammogram.
Breast ultrasound
Together with mammography, breast ultrasound is the first-level test for the early detection of breast cancer.
It is a non-invasive test that does not require the use of ionising radiation.
It can be performed from a young age and is increasingly being requested together with mammography by doctors as a complementary test.
It is important for the general population to be aware that mammography and ultrasound are complementary tests and not substitutes.
Ultrasound is particularly useful for detecting lesions in breasts with a high glandular component, such as in dense juvenile breasts.
It is painless and has no contraindications; it is preferable to perform it 5-10 days after menstruation due to the breast’s lower sensitivity.
If the doctor after the test is performed deems it appropriate, the patient may be asked to follow up at a later date: this should not cause anxiety for the patient because the absence of ionising radiation makes this instrument absolutely safe.
With ultrasound it is also possible to assess the galactophore ducts and thus any ectasia, papillomas or presence of intraductal material and the axillary lymph nodes.
From the age of 30 it is advisable to have an ultrasound every two years; in the case of a family history of breast cancer, check-ups will have to be more frequent and it will be up to the specialist to determine the timing.
After the age of 40, an annual mammogram is advisable, preferably combined with an ultrasound scan, especially in the case of high breast density.
The integration of these two methods, combined with the clinical assessment of the breasts by the doctor performing the test, is today the most effective tool in the early detection of breast cancer, often at a stage that still benefits from conservative treatment, as well as the best way to continue the diagnostic process.
For this reason, it is important for women of all ages to be familiar with and aware of the tools at their disposal and their diagnostic potential.
Needle aspiration and biopsy for breast cancer diagnosis
When the presence of a lump or suspicious area is established, the next step is biopsy.
This consists of taking cellular material (cytological or histological) with different sized needles and submitting it to the anatomic pathologist to determine its benignity or malignancy and possible prognostic factors.
It can be performed under radiological (stereotactic) or ultrasound guidance depending on the type of lesion.
The procedure is minimally painful and therefore does not require the use of anaesthetic drugs, only ice.
The result is delivered by a breast doctor who will explain, in the event of a negative result, the timing of subsequent routine check-ups, while discussing treatment options in the event of a positive finding of neoplastic cells, depending on the type of tumour.
Sometimes it may happen, especially in the case of very small lesions, that the material taken is inadequate, in which case you will be called back for a new sample, a new test or a short-term follow-up.
Usually the only complication is a haematoma at the sampling site.
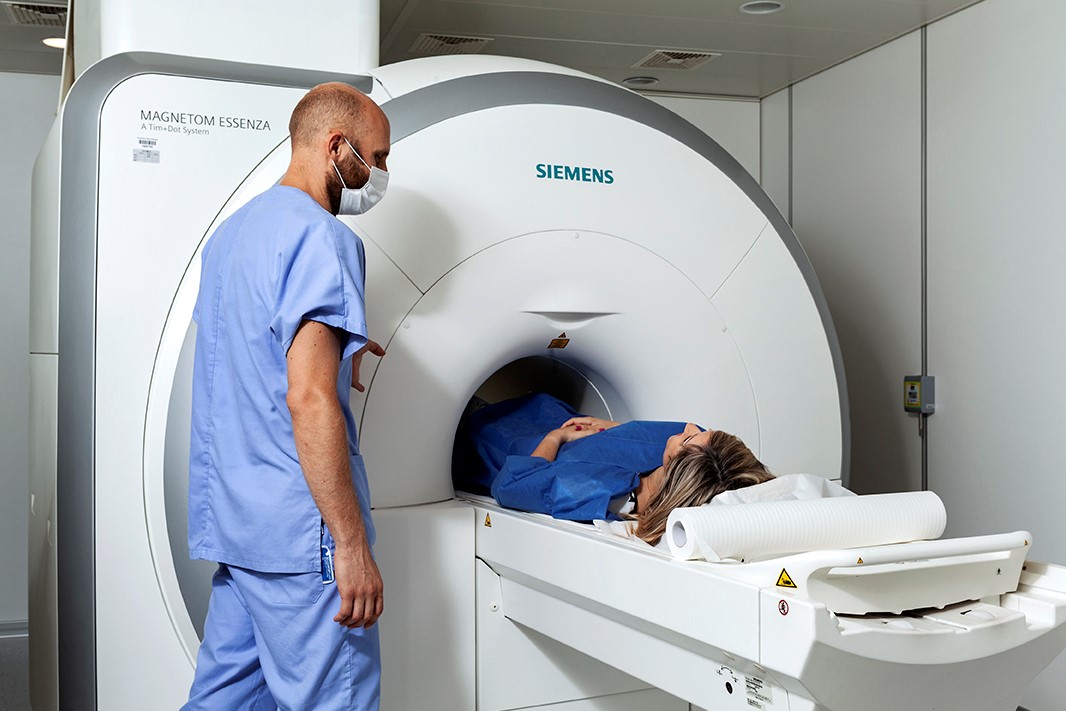
Magnetic resonance imaging
This is a non-invasive diagnostic test that is performed on machines with a high magnetic field (1.5 T or 3T) and allows the mammary gland and lymph nodes to be studied.
It does not use ionising radiation and is therefore risk-free for the patient and can be performed at any age.
It can be performed with or without contrast medium: in the first case for the study of unknown primary carcinoma syndrome when lymph node metastases have been found, but the primary tumour is not detectable in the first level tests; for staging already confirmed lesions of which multifocality/multicentricity is suspected; for evaluation of efficacy after neoadjuvant therapy, or in the case of women with high genetic risk (BRCA1 OR BRCA2 mutated) and significant family history; in the second for evaluation of the integrity of prosthetic implants for aesthetic purposes or after mastectomy.
The patient is placed in a prone position on the MRI couch with her arms along her body and her breasts resting on the dedicated coils.
The test takes about 15 minutes.
For women of childbearing age, it is preferable to perform the test within two weeks of the first day of their menstrual cycle.
It is necessary to fill out a questionnaire beforehand regarding the possibility of metal objects in the body (splinters, prostheses, pacemakers, etc.), which will then be assessed for suitability.
It is also important to remove all clothing with metal parts, jewellery, piercings, clothes pegs, contact lenses, glasses, cosmetics and any object that could potentially be metal.
In the case of a test with contrast medium, it is necessary to fast for at least four hours and take a creatinine test not older than three months.
In addition, it is important to remember to bring previous tests with you so that they can be compared.
All tests and procedures described require a verbal or written informed consent.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Breast Cancer: For Every Woman And Every Age, The Right Prevention
Transvaginal Ultrasound: How It Works And Why It Is Important
Pap Test, Or Pap Smear: What It Is And When To Do It
Mammography: A “Life-Saving” Examination: What Is It?
Breast Cancer: Oncoplasty And New Surgical Techniques
Gynaecological Cancers: What To Know To Prevent Them
Ovarian Cancer: Symptoms, Causes And Treatment
What Is Digital Mammography And What Advantages It Has
What Are The Risk Factors For Breast Cancer?
Breast Cancer Women ‘Not Offered Fertility Advice’
Ethiopia, The Minister Of Health Lia Taddesse: Six Centers Against Breast Cancer
Breast Self-Exam: How, When And Why
Fusion Prostate Biopsy: How The Examination Is Performed
CT (Computed Axial Tomography): What It Is Used For
What Is An ECG And When To Do An Electrocardiogram
MRI, Magnetic Resonance Imaging Of The Heart: What Is It And Why Is It Important?
Mammary MRI: What It Is And When It Is Done
What Is Needle Aspiration (Or Needle Biopsy Or Biopsy)?
Positron Emission Tomography (PET): What It Is, How It Works And What It Is Used For
CT, MRI And PET Scans: What Are They For?
MRI, Magnetic Resonance Imaging Of The Heart: What Is It And Why Is It Important?
Urethrocistoscopy: What It Is And How Transurethral Cystoscopy Is Performed
What Is Echocolordoppler Of The Supra-Aortic Trunks (Carotids)?
Surgery: Neuronavigation And Monitoring Of Brain Function
Robotic Surgery: Benefits And Risks
Refractive Surgery: What Is It For, How Is It Performed And What To Do?
Single Photon Emission Computed Tomography (SPECT): What It Is And When To Perform It
What Is An ECG And When To Do An Electrocardiogram
MRI, Magnetic Resonance Imaging Of The Heart: What Is It And Why Is It Important?
Mammary MRI: What It Is And When It Is Done
Mammography: How To Do It And When To Do It
Pap Test: What Is It And When To Do It?


