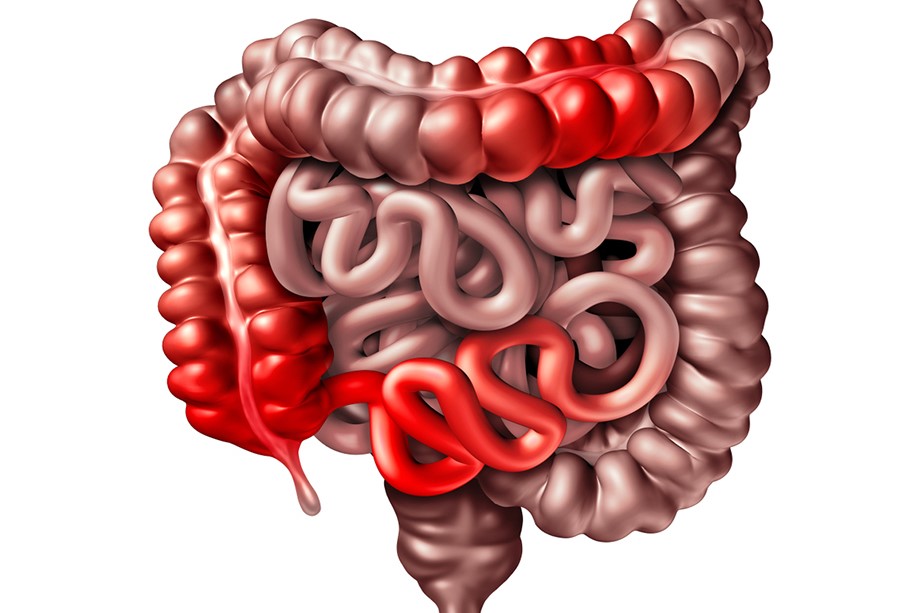
Chronic inflammatory bowel diseases: let's talk about ulcerative rectocolitis (UC) and Crohn's disease (MC)
The term chronic inflammatory bowel disease encompasses two diseases that are similar in many respects but still retain their individuality: ulcerative rectocolitis (UC) and Crohn’s disease (CD)
The former is characterised by a condition of inflammation of the intestinal wall of the colon, i.e. the end tract of the intestine, the latter predominantly by inflammation of the ileum (i.e. the part of the intestine between the stomach and the colon), but sometimes also of the colon itself or of any other tract of the digestive system.
Their course is typically chronic, characterised by acute phases often interspersed with more or less long periods of remission of symptoms.
They mostly occur in young people between the ages of twenty and forty, and sometimes more than one person in a family group may be affected.
In Europe (other regions of the world and other ethnic groups have a much higher incidence of MICI) overall, the two diseases affect approximately 10-15 people per 100,000 inhabitants, with no gender preference, although MC is slightly more frequent in women.
No precise causes are recognised for either disease, although for years infectious factors (viruses or bacteria), hereditary factors, stress, etc. have been suspected, without any of these having yet been confirmed.
Chronic inflammatory bowel disease: how do I notice it?
The symptoms with which both diseases present themselves are very similar and do not always, on their own, allow the doctor to make an accurate diagnosis of one or the other disease.
Abdominal pain is almost always the prevailing symptom; it may be diffuse or localised in certain areas depending on which intestinal tracts are most inflamed. Fever, emaciation, lack of appetite and tiredness are also often present.
There is almost always diarrhoea or at any rate stools of a soft consistency, with evident presence of blood and mucus; discharges mostly occur several times a day, especially in the more acute phases of the illness.
Sometimes there is joint pain, sometimes, though rarely, eye, liver or skin complications.
Tests for chronic inflammatory bowel disease
Laboratory examinations show the typical alterations present in most inflammatory diseases of different origins, e.g. increased white blood cells, anaemia, elevated ESR and CRP values, increased fibrinogen and alpha 2 fraction in the protein electrophoretic picture.
However, the laboratory can only in principle suggest the diagnosis of MICI, whereas the examinations required to make a precise diagnosis are instrumental, in particular radiological (enemas) and endoscopic (colonoscopy and push or retrograde ileoscopy).
In the case of the schism, the radiopaque contrast medium can be introduced through the anus and then dilated with air if one wants to study the colon (double-contrast colon schism), or through a nasal tube that descends into the stomach if one wants to study the parts of the intestine (small intestine, etc.) typically affected by Crohn’s disease (double-contrast small intestine schism).
Endoscopic examinations
Colonoscopy, which is carried out by introducing, after suitable preparation with enemas or special laxatives, the endoscope from the anus, is especially important in the diagnosis of RU.
If the patient tolerates the examination well, the colonoscopy can be conducted up to the last loops of the small intestine (in which case it is also called retrograde ileoscopy).
Another endoscopic examination is the push-through ileoscopy, i.e. with a thin, long instrument similar to a gastroscope one is able to explore, starting from the mouth, the stretch of intestine known as the small intestine most typically affected by MC.
Ultrasonography, a very well-tolerated and easily repeatable investigation, can also be used to diagnose inflammatory bowel disease, both to identify the affected tracts and to monitor them over time.
What to expect
The course of both diseases is typically chronic, characterised by more or less short periods (days or weeks) of even very severe flare-ups, alternating with very long phases (even years) of absolute remission of symptoms and inflammation.
In any case, in the vast majority of cases, patients have more than one episode of flare-up during their lifetime, while complete recovery very rarely occurs after a single episode.
Unfortunately, in spite of medical therapies, it is possible for both diseases to develop even serious, though fortunately very rare, complications: in order of rarity, the onset of stenosis (narrowing of the calibre of a stretch of intestine affected by severe inflammation, with the possibility of this stretch being occluded), perforation of the wall, massive haemorrhages, forms of considerable magnitude known as fulminant forms, so-called toxic forms with paralysis of the intestine (toxic megacolon), the onset of tumours in the regions most affected by the inflammatory process and in patients with a longer history of the disease.
Moreover, as already mentioned, it is possible for MC in particular to involve other apparatuses or organs at the same time, thus leading to complications in the eye, skin, liver, kidneys and joints.
Chronic inflammatory bowel disease: what to do
Once the diagnosis of MICI has been suspected or made, it is preferable to turn to specialised doctors and facilities for therapy and subsequent periodic checks.
Basically, we must distinguish between two different therapeutic moments.
In the most acute phase of the disease, hospitalisation is almost always necessary in order to be able to implement any necessary therapeutic and supportive measures.
It is usually necessary to impose fasting on the patient, and then intravenous nutritional and fluid support will be needed.
In some cases, haemotransfusions may also be necessary; in other cases, fortunately rare at the beginning of the disease, the clinical picture may be so severe that specialists may advise the patient to be referred to the surgeon in order to carry out the removal of more or less long stretches of intestine irreparably affected by inflammation.
Outside these periods of more acute inflammation, periods of remission of symptoms or at least of lesser intensity can be safely treated at home by the patient, with periodic outpatient check-ups.
The cornerstones of medical therapy, both in the acute phase and in those in remission, involve the use of anti-inflammatory drugs (mostly cortisone), drugs that modify the body’s immune response (salazopyrin and aminosalicidic acid and derivatives), sometimes even immunosuppressive drugs (such as azathioprine or cyclosporine) or particular types of antibiotics.
Logically, all the therapeutic baggage must be used by the specialist with different dosages, combinations of the various drugs and ways of administering them (oral, enemas, intramuscular, etc.) depending on the stage of the disease.
Very often it is necessary during remission phases to prolong medical therapy, even for very long periods, to prevent or limit flare-ups.
Advice
No particular dietary restrictions are necessary during the remission periods, but a particularly varied diet with foods that are well digestible and tolerated by the patient is recommended.
Smoking, which worsens the course of MICI, should be discouraged, and alcoholic beverages should be moderated.
Psychophysical stress and states of anxiety were for a long time thought to be in some way conducive to the onset of mycosis or its flare-ups, but their role has now been greatly reduced.
During therapy, women mostly retain normal fertility, which is somewhat reduced in men when treated with sulfasalazine.
In the event of an established or suspected pregnancy, a specialist should be consulted for any changes in medical therapy.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Crohn’s Disease: What It Is And How To Treat It
Psoriasis: What It Is And What To Do
Wales’ Bowel Surgery Death Rate ‘Higher Than Expected’
Irritable Bowel Syndrome (IBS): A Benign Condition To Keep Under Control
Colitis And Irritable Bowel Syndrome: What Is The Difference And How To Distinguish Between Them?
Irritable Bowel Syndrome: The Symptoms It Can Manifest Itself With
Crohn’s Disease Or Irritable Bowel Syndrome?
USA: FDA Approves Skyrizi To Treat Crohn’s Disease
Crohn’s Disease: What It Is, Triggers, Symptoms, Treatment And Diet
Gastrointestinal Bleeding: What It Is, How It Manifests Itself, How To Intervene
Faecal Calprotectin: Why This Test Is Performed And Which Values Are Normal
What Are Chronic Inflammatory Intestinal Diseases (IBD)?
Chronic Inflammatory Diseases: What They Are And What They Involve


