Understanding the Differences Between Rapid-Action and Long-Acting Insulins
Introduction
Insulin is essential in diabetes management, but not all insulins are the same. Specifically, rapid-action and long-acting insulins play different roles in blood sugar control. This article explores the key differences between these two forms of medication, providing essential information for patients and healthcare professionals.
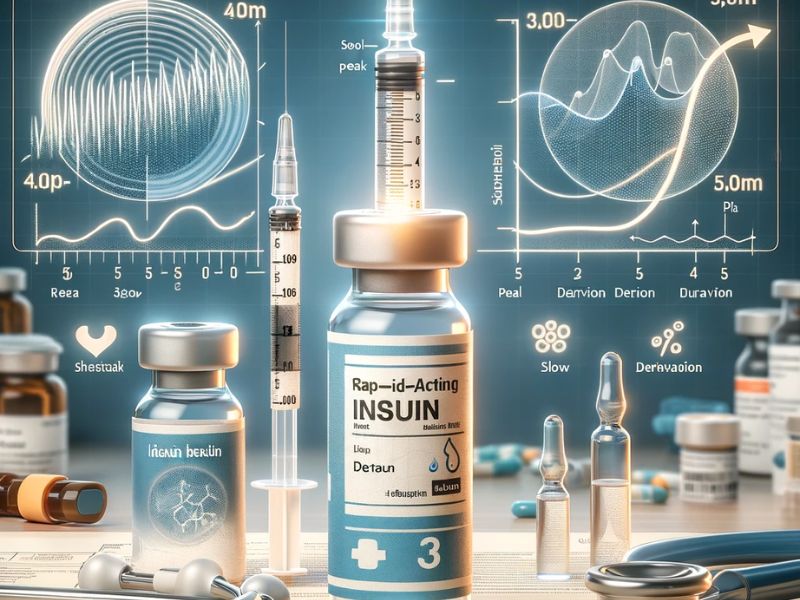
Rapid-Action Insulin
Rapid-action insulin, as the name suggests, starts working quickly after injection. Typically, this type of product begins to take effect within 15 minutes of injection, reaches its peak effectiveness in an hour or two, and continues to work for about two to four hours. It is often used to manage the post-meal increase in blood sugar, being injected shortly before or after eating.
Long-Acting Insulin
On the other hand, long-acting insulin acts more slowly but provides a steady and prolonged blood sugar control. This insulin starts working a few hours after injection and can last up to 24 hours. It provides a basal level of insulin, helping to maintain stable blood sugar throughout the day and night, and is often injected once or twice a day depending on the patient’s needs.
Choice and Usage: Balancing Risks and Benefits
The choice between rapid-action and long-acting insulin requires a careful assessment of risks and benefits based on various factors such as the type of diabetes, diet, lifestyle, and individual preferences. Rapid-action insulin is effective in managing rapid post-meal blood sugar spikes but requires careful meal planning to avoid hypoglycemia, a dangerous condition characterized by excessively low blood sugar levels. On the other hand, long-acting insulin offers more stable blood sugar control, reducing the risk of unexpected fluctuations but may be less flexible in adapting to changes in diet or physical activity.
Close collaboration with healthcare professionals is crucial in determining the most suitable insulin therapy, considering both the benefits of maintaining stable blood sugar levels and associated risks, such as hypoglycemia, especially during the night. Patients should be informed about warning signs of hypoglycemia and how to manage it. Understanding the differences between these insulins and open communication with healthcare professionals can help optimize diabetes control and improve the quality of life for patients while reducing the risk of short- and long-term complications.
Sources


