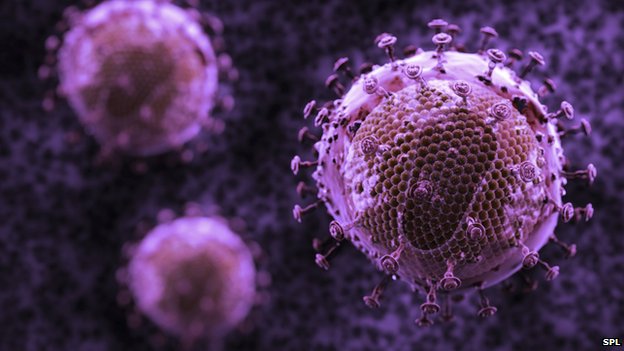
Covid and HIV: 'Monoclonal antibodies for the cures of the future'
Covid and HIV, the turning point is in monoclonal antibodies? New therapeutic horizons were discussed during the 13th edition of the Icar Congress – Italian Conference on Aids and Antiviral Research
Science at work on HIV and Sars-CoV-2: new solutions on the horizon after the extraordinary progress of recent months, and monoclonal antibodies are the protagonists
If for Covid vaccines have made it possible to reduce contagions and serious cases of the disease, for some years now HIV can be considered a chronic infection thanks to the advent of highly effective antiretroviral therapy that allows the control of viral replication and the consequent virological suppression, synthesised in U=U, Undetectable=Untransmittable: HIV is not transmitted if the viremia of the HIV-positive partner is no longer detectable in the blood, thanks to the correct intake of effective antiretroviral therapy.
The new therapeutic horizons offer further insights: for both HIV and Covid, further solutions may lie in monoclonal antibodies.
This is one of the ideas emerging from the 13th edition of the Icar Congress – Italian Conference on Aids and Antiviral Research, being held in Riccione from 21 to 23 October.
HIV AND COVID-19, THERAPEUTIC APPROACHES WITH MONOCLONAL ANTIBODIES
Monoclonal antibodies have become one of the most important pharmaceutical products also in the infectious field: the first monoclonal in this sense was used for the respiratory syncytial virus, then for Clostridium difficile; recently studies and the first applications for HIV and Covid have begun.
In the recent pandemic, this therapeutic approach proved crucial in preventing the disease triggered by Covid from degenerating into its most serious forms.
In HIV, there is a monoclonal antibody, ibalizumab, which has passed phase 3 trials.
It has already been approved by the Fda and Ema and is in the process of being approved by Aifa these very days, and will soon be available in our surgeries.
“This monoclonal antibody attaches itself to CD4 cells, preventing the virus from entering the cell,” explains Prof. Anna Maria Cattelan.
This therapeutic approach has been designed for patients with a long history of antiretroviral therapy and virological failure.
The data at 96 weeks of treatment indicate that even in multi-failed subjects there was a virological response in 56% of cases; I would say this is an important result for future developments of the molecule.
This is only the beginning, as these monoclonal antibodies could also be used in other contexts, such as in initial therapy and even in the prevention of HIV.
A study published this year in the New England Journal of Medicine on the prevention of HIV infection on more than 4,000 subjects at high risk of infection, although it did not prove effective in achieving this ambitious result, represented an important ‘proof of concept’, both for the development of future vaccines, and for the planning of further future studies that will have to involve the simultaneous combination of several monoclonal antibodies capable of attacking the virus definitively.
A decade is certainly beginning that will see the development of many advanced therapeutic strategies, including gene therapy.
DAILY PROTECTION? VISIT THE SUISSE RESSOURCES BOOTH AT EMERGENCY EXPO
MONOCLONAL ANTIBODIES: LONG COVID AND HIV AT THE ROOT OF PREMATURE AGEING, THE IMPACT OF “GEROSCIENCE
Among the many similarities that characterise Covid and HIV, research is gaining ground on the effect that both viruses have on the ageing of the individual, understood as a condition of fragility with respect to the accumulation of deficits in the course of our lives.
“HIV is a refined model of the accentuation and acceleration of the ageing phenomenon,” emphasises Prof. Giovanni Guaraldi, infectious diseases physician at the Azienda Ospedaliero-Universitaria di Modena and Associate Professor at the local University.
In the last year, among the effects of the pandemic, we have also observed the Post Acute Covid Syndrome – Pacs, often simply called Long Covid, which is also a phenomenon of ageing of the person, as can be seen from the empirical evidence in many patients who feel changed after Covid.
HIV and Pacs are united by this biological mechanism of acceleration of the ageing phenomenon with progression of frailty.
It is precisely on the subject of ageing that a new science, geroscience, has been emerging for some years now, according to which ageing is a disease that should be tackled by means of early diagnosis in order to promote targeted interventions through senolytic drugs, which can kill ageing cells, and senomorphic drugs, which can modify cellular ageing.
As Hiv and Covid are two ageing diseases, it is interesting to understand the geroscience approach to these diseases.
However, HIV can already be considered as a model where geroscience is applied, as antiretroviral therapy actually has a senomorphic function.
HIV AND SARS-COV-2 IN THE LABORATORY
Covid-19 has made infectious scientists relive the nightmare they have experienced in recent decades when faced with HIV.
Yet the two infections showed profound differences, which are mainly reflected in the laboratory tests.
Sars-CoV-2 and HIV differ in terms of the importance of the quantitative aspect, the relationship between infection and contagiousness, the monitoring of immunity, and the role of variants,” Prof. Maria Rosaria Capobianchi points out.
In Covid, which is an acute infection, the importance of the quantitative aspects of viral load, which is crucial for monitoring infection in HIV, a chronic infection, has been greatly reduced.
If an HIV patient achieves a quantitative reduction in viral load, he or she may no longer be infectious, as stated in the U=U principle; in Covid, on the other hand, there may be prolonged persistence of the viral genome in the respiratory tree, but this does not correspond to persistent infectiousness.
In addition, the concept of immunity changes: in HIV it is not a sign of recovery, but of lifelong infection, whereas in Covid the presence of antibodies is evidence of having encountered the virus and having overcome the infection.
Antibodies are also a key parameter for the assessment of vaccine-induced protection, in model populations from which information on the duration and extent of protection can be drawn, so that flexible and timely strategies for vaccination policies can be designed.
Many tools for measuring immunity, both natural and vaccine-acquired, are currently available.
However, the antibody levels that correspond to the state of protection are still unclear, and many laboratories are working on comparing the different immunometric methods with the biological test that measures the ability to neutralise virus infectivity.
In fact, this test, due to its complexity, cannot represent the routine standard, and for this reason, more accessible and simple instruments must be identified for everyday applications. In addition, the most recent data also focus on cellular immunity, which seems to have a longer duration than antibody immunity.
Cellular immunity also seems to be less affected by viral variability.
Linked to this, it must be said that on the Covid side there is a great deal of attention for virus variants that could frustrate the protection of vaccine-induced immunity.
In HIV, the experience we have gained over the last 40 years has taught us that mutations are important in a different context, mainly linked to the effectiveness of antiretroviral drugs’.
Read Also:
Sanofi Pasteur Study Shows Efficacy Of Co-Administration Of Covid And Influenza Vaccines
WHO: ‘Pandemic Will Continue Unless Vaccines Are Distributed To Poor Countries’
Italy, Study With CNR: Eugenol Antiviral Potential Against Covid-19


