Crohn's disease: symptoms, complications and treatment
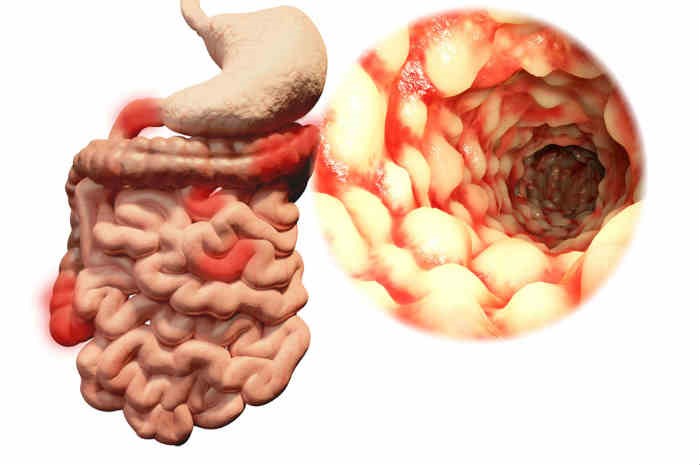
Crohn’s disease is a chronic inflammation that can theoretically affect the entire alimentary canal, from the mouth to the anus, but is mainly localised in the last part of the small intestine called the ileum (ileitis) or in the colon (colitis) or in both (ileo-colitis)
In the affected intestinal tracts there is inflammation, swelling and ulceration affecting the entire intestinal wall.
How many people in Italy are affected by Crohn’s disease or ulcerative rectocolitis?
At present there is no National Registry of C.I.M., nor reliable data.
However, it is estimated that in Italy there are at least 100,000 people affected by chronic inflammatory bowel disease.
With regard more strictly to Crohn’s disease, it mainly occurs in youth (20/25 years) and in old age (65 years) but cases are not rare in children and adolescents either.
Moreover, this disease is mainly present in countries with a high level of industrial development while it is rare, if not absent, in Third World countries.
What are the symptoms of Crohn’s disease?
Although there are variations from case to case, abdominal pain is predominant in Crohn’s disease (sometimes, if acute, it can mimic an appendicitis attack) associated with diarrhoea and sometimes fever.
The pain is localised in the umbilicus or right side of the abdomen and often occurs after meals.
Joint pain, decreased appetite or weight loss may also appear, although more rarely.
Other early signs of the disease may be the presence of anal fistulas (abnormal openings between the intestine and the skin surface, near the anus) and abscesses.
What are the causes?
The causes are still unknown, which limits medical therapy to the use of drugs that control the inflammation.
It can certainly be said, based on current scientific knowledge, that it is not a contagious disease, that it is not caused by food and that it is not psychosomatic (i.e. not caused by individual psychological factors).
Is Crohn’s disease hereditary?
It is not a hereditary disease in the strict sense of the term, as Mediterranean anaemia and haemophilia can be, which are considered genetic diseases, i.e. transmissible through chromosomes.
There is, however, some familial predisposition in the development of the disease; in fact, a number of patients (approximately 15/20%) have one or more close relatives affected by Crohn’s disease (or ulcerative colitis).
However, if a person has this disease, there is a low probability that an eventual child will contract it in turn.
Why is Crohn’s disease called a chronic disease?
Unlike an acute disease, such as influenza, which manifests itself with a short, sharp course and evolves with healing, a chronic disease such as Crohn’s disease does not heal permanently and can alternate between long periods of well-being and others in which symptoms are present.
Unfortunately, at least to date, we have no instrument that can predict with certainty a probable relapse, i.e. a flare-up of the disease, after medical treatment or surgery.
What are the complications of Crohn’s disease?
Complications of a disease can be defined by the events that make its clinical course more complex and troublesome.
In Crohn’s disease, both intestinal and extra-intestinal complications can occur.
Do complications affect all C.I.M. patients?
Absolutely not. They affect about 10/20% of patients.
The remaining 80/90% respond satisfactorily to medical therapy and have no complications.
What are intestinal complications?
Episodes of ‘intestinal obstruction’ (stenosis) are probably the most common intestinal complication.
These episodes are due to the fact that the inflammatory process can create narrowings of certain tracts of the intestine.
These narrowings are ‘unstable’ and can cause cramping, meteorism (gas formation), abdominal distention and sometimes even partial obstruction (sub-occlusion) or even complete obstruction of the intestinal flow (occlusion).
In the latter case, the symptoms described may be associated with nausea and vomiting.
Obstruction can occur most easily in the presence of undigested food, such as nuts or seeds, or clusters of fibre that prevent the passage of other material.
This is one reason why patients with Crohn’s disease who have stenotic areas should avoid foods with ‘coarse fibres’ that are difficult to digest.
If recurrent occlusive or sub-occlusive episodes occur, these strictures may be an indication for surgery.
Perforations’ (a subsequent cause of abscess) are another not uncommon complication in cases of very active disease.
Occasionally they may result in massive rectal bleeding; however, the bleeding is generally more gradual in nature.
Abdominal abscesses’ and ‘fistulas’ are also characteristic of Crohn’s disease (approximately 25% of sufferers) and are considered an extension of the same disease process.
An abscess consists of a cavity formed by tissue destruction.
A fistula is an abnormal communication that may develop from the abscess cavity to another intestinal area or to the skin or even to another intra-abdominal organ.
The symptoms of an abscess or fistula depend on their location.
An abscess usually causes fever, abdominal pain and localised distension and may resolve spontaneously or incision surgery may be necessary.
Treatment of a fistula requires the actual removal of the severely inflamed part of the intestine from which it originates.
In some cases, however, fistulas can be cured by combining medical therapy with bowel rest (suspension of oral feeding).
What are the extraintestinal complications in Crohn’s disease?
Many complications of Crohn’s disease are similar to those of ulcerative colitis.
Some are related to disease activity, while others seem to follow a relatively independent course.
Complications related to disease activity may affect the skin, mouth and eyes, as well as large joints.
What are systemic affections?
By ‘systemic affections’ we mean those problems that can arise at sites other than the intestine, i.e. where the disease is localised, and include
- inflammation of the joints – the prevalence of these diseases in people with Crohn’s disease is higher than in the same general population (e.g. ankylosing spondylitis, sacroiliitis, lower back pain);
- liver diseases: these are not frequent in Crohn’s disease, although liver tissue changes may occur;
- gallstones: in the presence of Crohn’s disease they may be related to malabsorption of bile acids from the terminal ileum, because it is inflamed or surgically removed. Such malabsorption causes an increased concentration of cholesterol in the bile, which leads to stone formation;
- kidney stones: if the terminal ileum is inflamed or removed, there is malabsorption of fats which, by binding with calcium, favour the absorption of oxalate, which is the main constituent of kidney stones (calcium oxalate).
What is the medical treatment of Crohn’s disease?
There is acute phase therapy in which aminosalicylates ‘(5-ASA)’ ‘cortisone’ or ‘antibiotics’ are used, and remission maintenance therapy in which ‘(5-ASA)’ or, in severe cases, ‘(6-Mercaptopurine)’ (immunosuppressant) is used.
At present, therapy to prevent relapse, i.e. flare-ups in operated patients, may also be recommended.
It consists of starting 5-ASA immediately after the operation, which appears to lengthen the disease’s remission time.
Recently, a new anti-inflammatory drug, whose active ingredient is called Infliximab (currently in ‘band H’, i.e. only available at hospital level), has also been placed on the market in Italy.
It is a monoclonal antibody (anti-TNF), whose action is directed at blocking the cytokine (mediator of inflammation) alpha-TNF, involved in the mechanisms triggering the inflammatory process of Crohn’s disease.
The indications are as follows: treatment of active, severe Crohn’s disease in patients who have not responded to cortisone and/or immunosuppressant therapy; treatment of fistulising Crohn’s disease, which has not responded to an adequate course of conventional therapy.
What is the prognosis of Crohn’s disease?
The outlook is highly variable and depends on many factors including:
- location and extent of the disease
- complications;
- individual response to treatment.
There are patients who present with minor problems.
These may have intermittent symptoms of abdominal pain and must be careful with their diet to avoid foods that may increase their discomfort.
Some require constant treatment with high doses of cortisone and other drugs to control disease activity.
Others may require multiple surgeries to treat frequent intestinal obstructions.
Still others may undergo a single operation for ‘ileitis’ and never have major problems again.
Most patients are, however, in an intermediate situation and lead a healthy life, with no need to follow a diet and take medication as needed.
As is well known, there is no problem in wanting to start a family.
Men with Crohn’s disease are usually fertile, although in rare cases the taking of particular medication may give rise to transient alterations in the spermatozoa.
Women can become pregnant without complications, provided conception occurs during a period of remission.
It has also been shown that the drugs commonly used to control the symptoms are harmless for both mother and child.
Although there is a greater likelihood of Crohn’s disease within a family in which there is an already affected member, there is no proven possibility of one family member passing it on to another.
The remote possibility of a child developing the disease is not sufficient to prevent a couple wishing to have children from doing so.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Crohn’s Disease: What It Is And How To Treat It
Psoriasis: What It Is And What To Do
Wales’ Bowel Surgery Death Rate ‘Higher Than Expected’
Irritable Bowel Syndrome (IBS): A Benign Condition To Keep Under Control
Colitis And Irritable Bowel Syndrome: What Is The Difference And How To Distinguish Between Them?
Irritable Bowel Syndrome: The Symptoms It Can Manifest Itself With
Crohn’s Disease Or Irritable Bowel Syndrome?
USA: FDA Approves Skyrizi To Treat Crohn’s Disease
Crohn’s Disease: What It Is, Triggers, Symptoms, Treatment And Diet
Gastrointestinal Bleeding: What It Is, How It Manifests Itself, How To Intervene
Faecal Calprotectin: Why This Test Is Performed And Which Values Are Normal
What Are Chronic Inflammatory Intestinal Diseases (IBD)?
Chronic Inflammatory Diseases: What They Are And What They Involve


