Drug therapy for typical arrhythmias in emergency patients
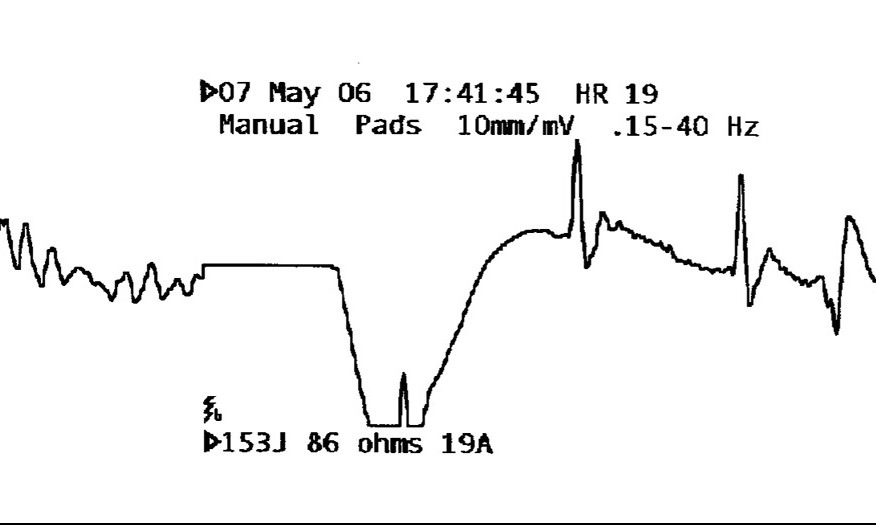
Atrial fibrillation (AF), atrial flutter, AV-nodal reentry tachycardia (AVNRT) with rapid ventricular response, atrial ectopic tachycardia and preexcitation syndromes (AVRT) sometimes combined with AF or ventricular tachyarrhythmias (VTA) are typical arrhythmias in emergency patients. Most frequently, the diagnosis of the underlying arrhythmia is possible from the 12-lead surface electrocardiogram, the physical examination and the response to manoeuvres or drugs. In unstable hemodynamics, immediate DC-cardioversion is indicated. Conversion of AF to sinus rhythm (SR) is possible using antiarrhythmic drugs. Amiodarone has a conversion rate in AF of up to 80%. A new drug for AF conversion is vernakalant. Acute therapy of atrial flutter (Aflut) in intensive care pts depends on the clinical presentation. It can most often be successfully cardioverted to SR with DC-energies less than 50 joules. In narrow complex tachycardia, if the patient is hemodynamically stable, treatment should start with vagal manoeuvre. If tachycardia persists and atrial flutter is excluded, use of adenosine (6 mg as rapid i.v. bolus) is suggested. Successful termination by vagal manoeuvre or adenosine indicates that it was AVNRT or AVRT. If there is no response to adenosine (even after a second bolus) a longer-acting drug (e.g. verapamil, diltiazem) is recommended. Drugs like procainamide, sotalol, amiodarone or magnesium are recommended for treatment of VTA pts. However, today only amiodarone is the drug of choice in VTA pts and also effective even in pts with defibrillation-resistant out-ofhospital cardiac arrest.
Dietrich Andresen, Hans-Joachim Trappe*
Klinik für Kardiologie, Allgemeine Innere Medizin und konservative Intensivmedizin, Vivantes Klinikum am Urban und im Friedrichshain, Berlin, Germany;
*Medizinische Klinik II (Kardiologie und Angiologie), Ruhr-Universität Bochum, Herne, Germany


