Dry eye syndrome: symptoms, causes and remedies
Dry eye is a pathological condition of the ocular surface that can lead to foreign body sensation, burning and other disorders that affect quality of life; the frequency of dry eye increases with age, in the presence of other diseases, especially rheumatic and hormonal, in association with various systemic therapies and exposure to environmental factors such as wind, air conditioning, excessive use of contact lenses and video terminals
What is dry eye
Currently, dry eye is defined as “a multifactorial disease of the ocular surface characterised by a loss of tear film homeostasis and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, inflammation, ocular surface lesions and neurosensory abnormalities play aetiological roles” (Dews II, 2017).
Dry eye is therefore considered a real disease, such that it affects the entire ocular surface system, consisting of the lacrimal apparatus, eyelids, cornea and conjunctiva.
This system is now considered a unitary structure, both anatomically and functionally, so that an abnormality in one of its components inevitably has repercussions on the others.
The fundamental characteristic that gives rise to dry eye is a change in the quantity and composition of tears, which become denser (tear hyperosmolarity) due to reduced production of the liquid component by the main lacrimal gland or excessive evaporation.
The increase in osmolarity in turn leads to damage of the epithelial cells of the conjunctiva and cornea, as well as the mucipare calyciform cells that produce the normal mucous component of tears, and induces an inflammatory reaction of the entire ocular surface.
These changes trigger a vicious circle that aggravates the dryness situation and leads to a chronicisation of the process, in the course of which the nerve pathways that convey impulses to the main lacrimal gland, which are necessary for normal tear fluid production, are also damaged.
Incidence of dry eye
Dry eye has a prevalence of about 15 cases per 100 people.
The incidence of the disease increases with age and in the female sex.
What are the causes and risk factors of dry eye?
It is considered a multifactorial disease, which is determined or favoured by multiple conditions, endogenous or environmental, some of them modifiable, others linked to individual characteristics.
- Age: it has been seen that the lacrimal glands lose part of their functionality over the years due to atrophy, reducing tear production or producing tears with an altered composition;
- female sex: it is more affected in all age groups, but especially coinciding with menopause, when the production of androgen hormones is reduced;
- environment: exposure to wind, dust, air conditioning, excessively dry or humid environments;
- excessive activity at video terminals;
- incorrect use of contact lenses;
- use of systemic drugs (antihistamines, psychotropic drugs, antihypertensives, anticholinergics, hormonal drugs, chemotherapy) or local drugs (glaucoma therapies, vasoconstrictors);
- systemic pathologies: rheumatic and collagen diseases, high blood pressure, diabetes mellitus, thyroid diseases;
- local pathologies: allergies, Meibomian gland dysfunction, insufficient closure or excessive opening of the eyelids, pterygium and other ocular surface changes.
Signs and symptoms of dry eye
Dry eye results in most cases in a foreign body sensation; other symptoms may be burning, stinging sensation, difficulty opening the eyes in the morning, vision disturbances.
In Sjogren’s syndrome and in cases related to other systemic diseases of the immune system, such as rheumatoid arthritis and other rheumatic forms, a feeling of dry mouth may be associated.
Characteristically, symptoms are accentuated in ventilated or excessively dry environments, in prolonged activity at video terminals and with the use of contact lenses.
The appearance of inflammation causes reddening of the conjunctiva; in some cases small mucus filaments may form.
Persistence of the complaints for more than three months indicates a tendency to chronicity.
Diagnosis of dry eye
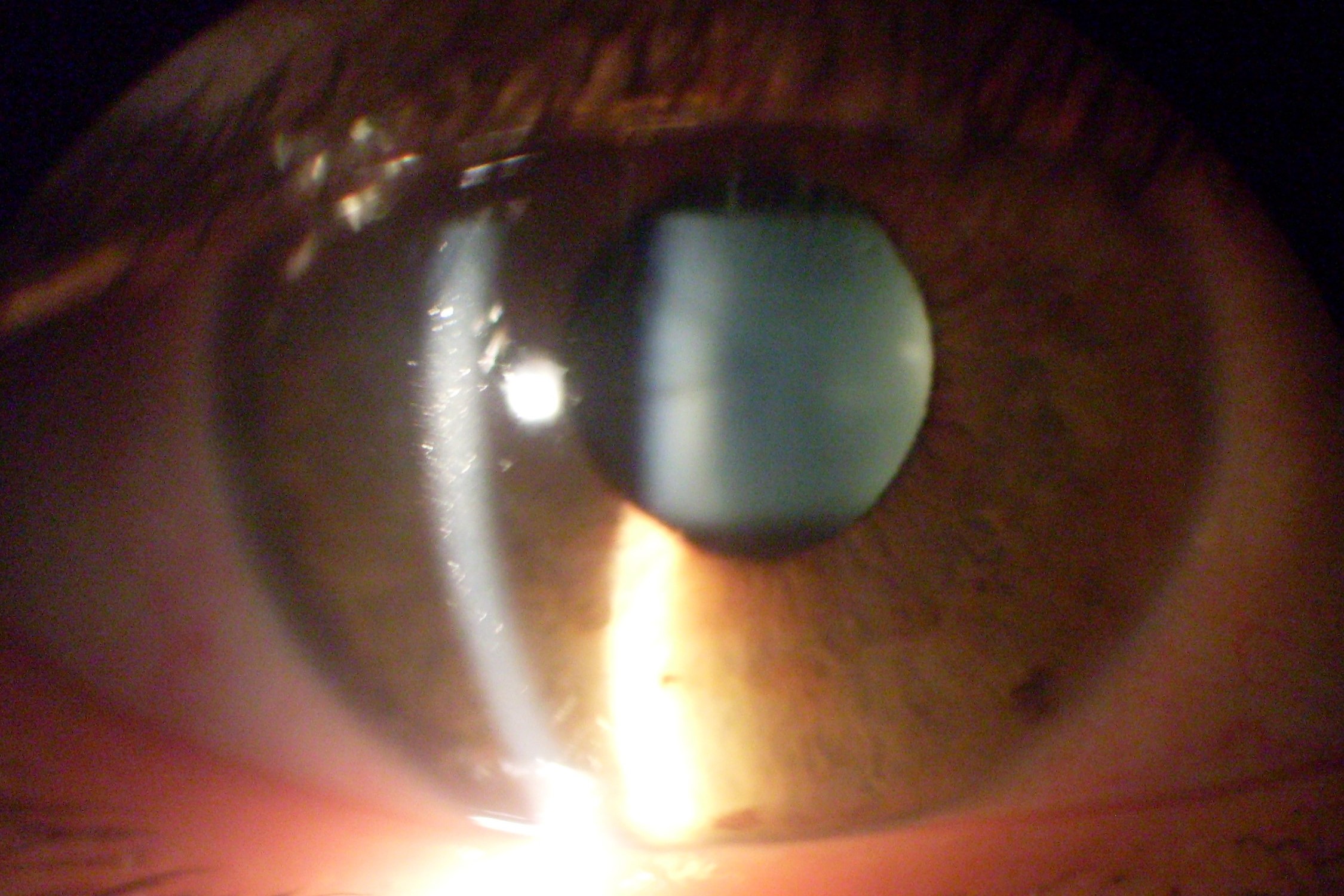
The diagnosis of dry eye is suspected during the ophthalmic examination based on the reported symptoms and observation of the ocular surface under the slit lamp and, more specifically, on the finding of a reduced thickness of the tear menisci, i.e., the layer of tears present between the eyelid edge and the surface of the eyeball.
The diagnosis is confirmed and clarified with certain tests:
- evaluation of the tear film break-up time, i.e. the lapse of time during which dry areas form on the surface of the cornea between one blink and the next; this examination can be carried out after instilling a fluorescent dye and observing the appearance of areas not covered by tears (dry spots) under the blue light of the slit lamp; the examination can also be carried out with special equipment that does not require the instillation of the dye;
- Schirmer test: evaluates the length of the soaked portion of a small strip of paper inserted into the conjunctival fornix, between the lower eyelid and the eye, over a certain period of time, usually 5 minutes;
- tear osmolarity test: allows a quantitative assessment of the degree of tear alteration;
- evaluation of the condition of the epithelial surface with the help of special stains (fluorescein, lissamine).
In the forms linked to inflammation of the eyelid glands of the meibomian, the disorders are most evident in the morning; engorgement of the excretory ducts located at the edge of the eyelids immediately behind the emergence of the eyelashes can also be observed.
When reduced tear production prevails, on the other hand, the tear meniscus appears much reduced and symptoms characteristically worsen in the course of the day.
How dry eye is treated
The treatment of dry eye varies depending on the stage of the pathology and the extent of the complaints.
In milder forms, it may be sufficient to avoid unfavourable environmental conditions and use tear substitutes based on hyaluronic acid, cellulose polymers or other substances such as trehalose, to be instilled at regular intervals, before symptoms recur.
As the dry condition persists, the appearance of epithelial cell suffering and inflammation requires the use of anti-inflammatory agents, usually mild cortisone, acting mainly on the surface, or cyclosporine, and re-epithelialising substances, in drops, gel or ointment.
The presence of inflammation of the eyelid glands (meibomitis), which is the most important cause of dry eye due to excessive evaporation, requires specific treatments, from simple moist warm compresses to the application of pulsed light devices.
The therapy must be set by the ophthalmologist, based on the characteristics and intensity of the clinical picture, and re-evaluated periodically to adapt it to the evolution of the pathology over time.
It is also necessary to rule out any concomitant allergic forms or superimposed infections.
Ultimately, a correct diagnostic framework is the prerequisite for a personalised and truly effective therapeutic strategy.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Red Eyes: What Can Be The Causes Of Conjunctival Hyperemia?
Autoimmune Diseases: The Sand In The Eyes Of Sjögren’s Syndrome
Corneal Abrasions And Foreign Bodies In The Eye: What To Do? Diagnosis And Treatment
Covid, A ‘Mask’ For The Eyes Thanks To Ozone Gel: An Ophthalmic Gel Under Study
Dry Eyes In Winter: What Causes Dry Eye In This Season?
What Is Aberrometry? Discovering The Aberrations Of The Eye


