Eye burns: what they are, how to treat them
Eye burns can occur after thermal or chemical injuries and can cause serious complications, including permanent blindness
Naturally, the care of an eye burn patient varies depending on the nature of the injury.
TREATMENT OF BURNS IN RESCUE OPERATIONS: VISIT THE SKINNEUTRALL BOOTH AT EMERGENCY EXPO
Thermal ocular burns
The blink reflex usually causes the eye to close in response to a thermal stimulus.
Thus, thermal burns tend to affect the eyelid rather than the conjunctiva or cornea.
Thermal burns should be carefully cleansed with sterile isotonic saline, followed by application of an ophthalmic antibiotic ointment (e.g. bacitracin twice/day).
Most thermal burns involving the conjunctiva or cornea are mild and heal without significant sequelae.
They are treated with oral analgesics (paracetamol with or without oxycodone), cycloplegic mydriatics (e.g., homatropin 5% 4 times/day), and topical ophthalmic antibiotics (e.g., bacitracin/polymyxin B ophthalmic ointment or ciprofloxacin 0.3% ophthalmic ointment 4 times/day for 3-5 days).
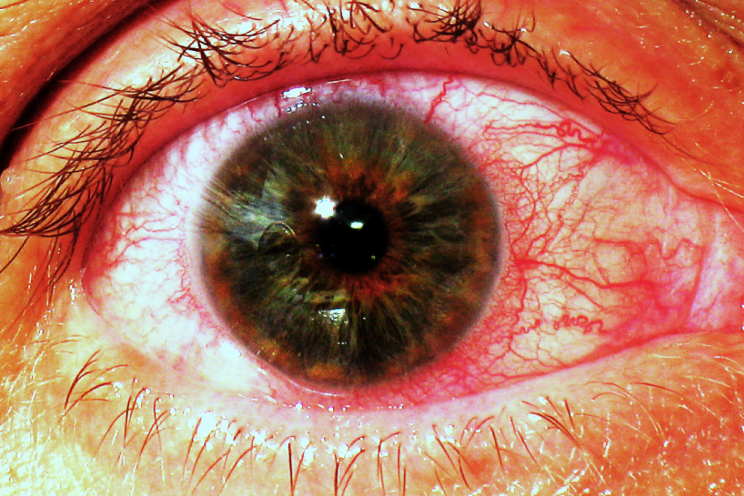
Chemical ocular burns
Chemical burns of the cornea and conjunctiva account for 11 to 22% of ocular trauma and can be severe, particularly when strong acids and alkalis are involved.
Alkali burns tend to be more severe than acid burns.
Chemical burns should be irrigated copiously as soon as possible.
The eye can be anaesthetised with a drop of 0.5% proparacaine, but irrigation should not be delayed and should last at least 30 min.
A borate buffer solution may be more effective than other irrigation solutions commonly used to correct intraocular pH, while a balanced saline solution (a sterile isotonic solution with a pH of 7.4) is better tolerated by patients who allow longer irrigation times.
But any saline solution or water can be used to avoid delays in irrigation.
Irrigation can be facilitated by using an irrigation lens placed under the eyelids, although this may cause more irritation to some patients than irrigation without the use of a lens.
In acid and alkaline burns, some experts suggest 1 to 2 L of irrigation; most experts recommend irrigation until the pH of the conjunctiva normalises (using pH indicators).
After irrigation, the conjunctival fornices should be examined for chemicals embedded in the tissue, and cleaned with a swab to remove trapped particles.
The upper fornices are exposed using double eyelid eversion (i.e., first everting the eyelid and then inserting a pad under the everted eyelid and lifting it until the fornix is visible).
Mild chemical burns are usually treated with topical ocular antibiotics (e.g., erythromycin ointment 0.5%) 4 times/day and cycloplegia if necessary to induce relief (e.g., cyclopentolate).
Since topical corticosteroids may cause corneal perforation after a chemical burn, they should only be prescribed by an ophthalmologist.
Topical anaesthetics should not be administered after the initial irrigation; intense pain can be treated with acetaminophen (paracetamol) with or without oxycodone.
If the patient’s renal function is not compromised, oral vitamin C (2 g 4 times/day in adults) can be used to promote collagen synthesis.
Oral doxycycline may also be used in appropriate patients to stabilise collagen, but both approaches should be carried out with the advice of an ophthalmologist.
Citrate eye drops, to decrease proteolytic activity, and platelet-rich plasma eye drops can also aid in healing, and should only be administered after consultation with an ophthalmologist.
Severe chemical burns require treatment by an ophthalmologist to save vision and prevent complications such as corneal scarring, eyeball perforation, and eyelid deformities; in addition to medical treatment, severe chemical burns may require surgical procedures.
Patients with severe reduced vision, avascular areas of the conjunctiva, or loss of conjunctival or corneal epithelium, demonstrated by fluorescein staining, should be seen by an ophthalmologist as soon as possible and no later than 24 hours after exposure.
Chemical iritis is suspected in patients with photophobia (profound eye pain with light exposure) that develops hours or days after a chemical burn, and is diagnosed by flare and white blood cells in the anterior chamber during slit-lamp examination.
Chemical iritis is treated by instilling a long-acting cycloplegic (e.g., a single dose of 2% or 5% homatropine or 0.25% scopolamine solution).
Bibliography:
-
Sharma N, Kaur M, Agarwal T, et al: Treatment of acute ocular chemical burns. Surv Ophthalmol 63(2):214-235, 2018. doi:10.1016/j.survophthal.2017.09.005
-
Baradaran-Rafii A, Eslani M, Haq Z, Shirzadeh E, et al: Current and upcoming therapies for ocular surface chemical injuries. Ocul Surf 15(1):48-64, 2017. doi:10.1016/j.jtos.2016.09.002
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Wound Infections: What Causes Them, What Diseases They Are Associated With
Patrick Hardison, The Story Of A Transplanted Face On A Firefighter With Burns


