Gardnerella vaginalis: causes, symptoms, diagnosis and treatment
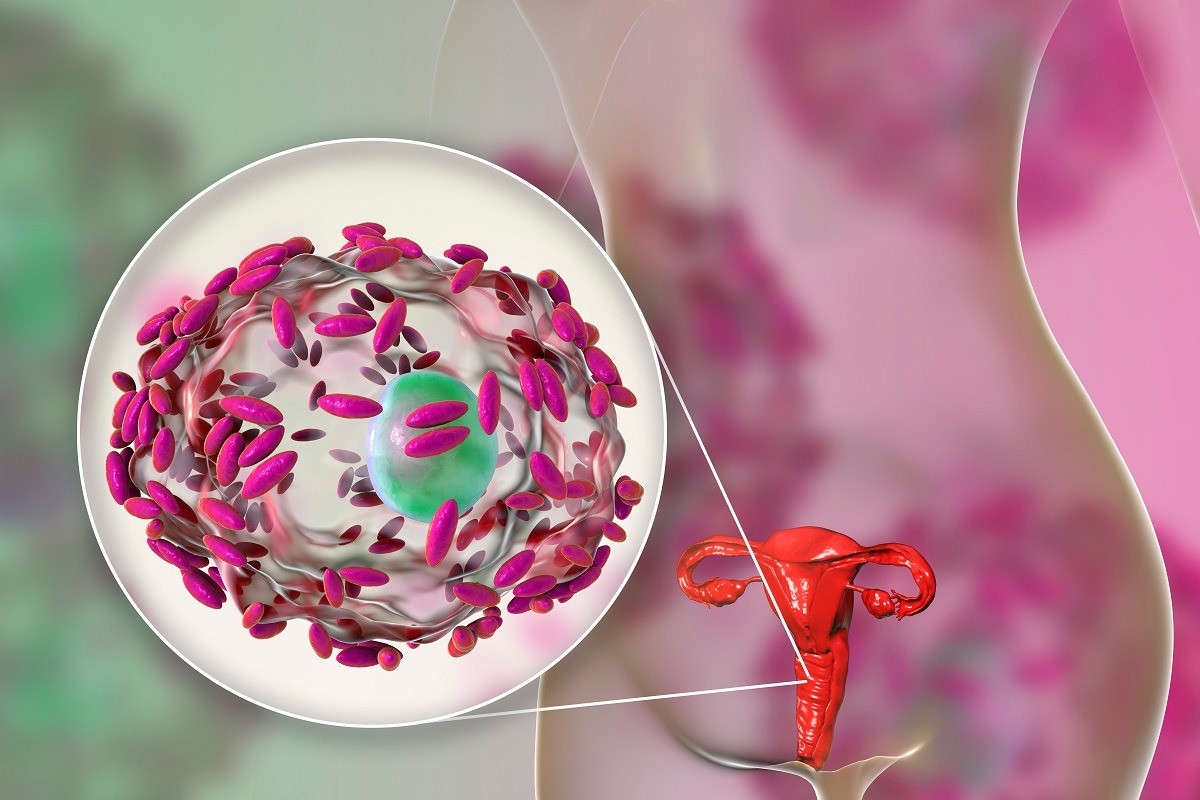
Gardnerella vaginalis is a gram-positive bacterium often responsible for vaginal infections (vaginosis). It is a potential pathogen that can cause serious damage to the vaginal mucosa if the normal vaginal pH (a safety and control factor towards potential pathogens) supported by lactobacilli, physiologically present in the normal vaginal flora, is disturbed
When the latter are reduced, the vaginal pH is raised, making the vaginal mucosa a breeding ground for Gardnerella, which can take root, reproduce uncontrollably and give rise to vaginosis.
As with everything that concerns health, only a specialist examination can confirm or not the presence of this infection, which is very frequent and should not be underestimated.
How is Gardnerella vaginalis diagnosed?
The diagnosis of Gardnerella in women is based on a gynaecological objective examination and certain techniques and laboratory tests.
The first sign that the patient reports is in most cases vaginal discharge with a characteristic fishy smell.
The gynaecologist can carry out the fishy odour test, which involves applying a drop of 10% potassium hydroxide in contact with the vaginal secretion in order to release the pungent odour typical of a Gardnerella infection.
Moreover, to further confirm the diagnosis, the gynaecologist can swab some desquamated cells and then microscopically check for the presence of the bacteria, which are usually abundant, analysing in particular the ‘clue cells’ (i.e. ‘clue cells’ that appear covered in bacteria under the microscope).
By taking a vaginal smear, it is then possible to carry out
- a microscopic analysis, which can identify the cells covered in bacteria that have precise characteristics that differ from the others
- a vaginal pH measurement above the normal value (3.8 to 4.5)
- Gram staining under the microscope
To be certain of being affected by Gardnerella vaginosis, it is therefore advisable to visit a gynaecologist, who will assess whether it is this type of infection or another problem, e.g. candida.
Symptoms
It can happen that a Gardnerella infection is asymptomatic (especially in men who carry the bacterium and in 30% of women in whom it is settled in the normal microbial flora).
In such a case, it is often not even necessary to proceed with specific treatment, but there are cases in which fairly straightforward symptoms occur, such as
- malodorous greyish-white discharge, especially when in contact with alkaline solutions (such as normal soap) with a particularly thick consistency, which increases near the menstrual cycle
- more or less intense burning sensation associated with urination, which could lead to confusion with cystitis;
- intimate irritation and itching, especially in association with excessively tight underwear or after sexual intercourse;
- pain during sexual intercourse.
In the presence of one or more of these symptoms, you should notify your gynaecologist so that he or she can make a timely and correct diagnosis.
Gardnerella vaginalis in pregnancy
Gardnerella can develop during pregnancy.
Women who are affected are at greater risk of premature birth or low birth weight babies (under 2.5 kg).
This can occur because, if left untreated, bacterial vaginosis produces such a proliferation of Gardnerella and consequent reduction in the amount of lactobacilli, that it can damage amniotic membranes and cause them to rupture.
It would be good practice for women who have had a history of premature birth or a low-birth-weight baby to be screened for Gardnerella infection during subsequent pregnancies
How is Gardnerella treated in pregnancy?
Pregnant women, with or without symptoms, at risk of preterm delivery must take antibiotics by mouth or in cream or ova for local application, with different modes of administration (and different doses) depending also on which trimester of gestation the patient is in.
Most frequently, ecosystem balancers are recommended because, in addition to having fewer side effects and being safer than antibiotics in pregnancy, instead of attacking the Gardnerella bacterium, they favour the proliferation of lactobacilli, which in turn inhibit the proliferation of the infection by restoring the physiological and correct pH of the vaginal microbiome.
Causes of Gardnerella vaginalis
The most common cause of Gardnerella is sexual transmission: the risk of developing bacterial vaginosis increases with increasing frequency and sexual promiscuity, not to mention that the slightly alkaline pH (7.4-7.6) of semen decreases vaginal acidity, encouraging the proliferation of pathogens. However, there are also other causes.
Among the most significant risk factors are:
- poor intimate hygiene or improper intimate hygiene (e.g. excessive use of douches or use of deodorants or aggressive soaps for intimate areas)
- use of mechanical contraceptives, such as IUDs;
- use of antibiotic drugs over a long period of time (which lower the immune defences and can weaken the lactobacilli);
- genetic predisposition.
Although most risk factors for Gardnerella are linked to ongoing sexual activity, even women who have never had vaginal intercourse can develop bacterial vaginosis.
Medications
Gardnerella is usually a type of infection that can be cured in a short time, but one should not underestimate the problem by expecting it to resolve quickly and without medication as there are numerous risk factors in neglecting a Gardnerella vaginosis.
In the long run, it can become chronic or degenerate into pelvic inflammatory disease that can even lead to infertility.
The treatment of Gardnerella involves the administration of antibiotics, usually locally (creams or ova).
The active ingredients most commonly used in products to combat Gardnerella vaginalis are:
- metronidazole, available in formulations for vaginal use (solutions, gels, creams and ova) and in formulations that can be taken orally (capsules) – not to be used during pregnancy;
- clindamycin, generally used topically (vaginal ova and creams).
Along with the use of antibiotic drugs, it is common for the doctor to suggest the use of vaginal douches with an acid content, which the woman should perform particularly at the end of sexual intercourse and after the end of the menstrual flow.
If necessary, the doctor may also suggest and prefer oral drug therapy.
The choice between one therapy or another is based solely on the doctor’s opinion according to the specific case to be treated.
In addition to taking antibiotics to eradicate the bacterial infection, the doctor may prescribe drugs based on acidifying agents that aim to restore the normal vaginal pH, which is higher than normal (tending towards basic) in the presence of ongoing Gardnerella. Finally, taking probiotics, either by mouth or locally, can be helpful in restoring vaginal bacterial flora.
As far as men are concerned, even though it is asymptomatic in most cases, in the event of a definite diagnosis of Gardnerella the treatment is almost the same as in women and it is not uncommon to resort to topical medication.
In fact, some gynaecologists consider it useful to proceed with specific treatment against Gardnerella for the patient’s partner as well, in order to prevent recurrences of the infection.
How to prevent it?
The best treatment for Gardnerella is prevention: adopting appropriate hygiene and behavioural measures, using barrier contraceptive methods and performing internal vaginal douches only when strictly necessary are the main guidelines for preventing this unpleasant bacterial infection.
Specifically, here is what should be done to prevent the appearance of Gardnerella
- cleanse intimate areas properly, using a soap with a physiological pH (4 or 5) and limiting intimate deodorants and internal cleansing;
- avoid wearing synthetic underwear, i.e. jeans and trousers that are too tight, as they retain moisture and heat. Continuous rubbing of the garment against the genitals can cause local irritation, which is why it is better to choose cotton;
- always use a condom during casual sex;
- avoid the shared use of towels and underwear;
- avoid wearing a wet swimming costume for a long time;
- follow a healthy, balanced diet by reducing sweets and simple sugars.
There are some cases in which bacterial vaginosis tends to relapse: relapses occur when there is difficulty in re-establishing the normal vaginal environment on its own after treatment.
In these cases, prevention is essential to avoid relapses.
As far as pregnant women are concerned, an important role in prevention is played by vitamin D.
In pregnancy, its deficiency triples the risk of bacterial vaginosis, so its values should be measured with a blood test and, if it is insufficient (i.e. below 30 ng/ml), a supplement should be used, with the right amount (daily, weekly or monthly).
Keeping vitamin D levels under control helps to avoid serious obstetrical and neonatal risks and bacterial vaginosis.
Lastly, probiotics can also help fight Gardnerella because, if used during pregnancy, they should enable the ‘friendly’ vaginal bacterial flora to be restored through the application in the vagina of preparations containing lactobacilli, in the form of ovules or tablets.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Gardnerella Vaginalis Vaginosis: Symptoms, Diagnosis And Treatment
Vaginal Yeast (Candidiasis): Causes, Symptoms And Prevention
Chlamydia, Symptoms And Prevention Of A Silent And Dangerous Infection
Vulvodynia: What Are The Symptoms And How To Treat It
What Is Vulvodynia? Symptoms, Diagnosis And Treatment: Talk To The Expert
What To Eat With Endometriosis
Gender Medicine, What It Is And What Consequences Endometriosis Has
Urinary Incontinence: The Causes And An Overview Of Cures And Treatments
Endometriosis Cyst: Symptoms, Diagnosis, Treatment Of Endometrioma
Endometriosis, The Characteristic Symptom Is Pain
Vulvar Pain: Symptoms, Diagnosis, Treatment And Prevention
Dysmenorrhoea: Definition And How To Treat It
Vaginal Candida, Symptoms And How To Treat It
Vaginal Candida: Causes, Symptoms And Prevention
Candida: Definition, Symptoms, Diagnosis And Treatment Of Vaginal Infection
Colposcopy: How To Prepare, How It Is Performed, When It Is Important
Cystitis: Symptoms, Causes And Remedies
Cystitis, Antibiotics Are Not Always Necessary: We Discover Non-Antibiotic Prophylaxis
Polycystic Ovary Syndrome: Signs, Symptoms And Treatment
Female Cystitis, How To Deal With It: Urological Perspectives
How Does Cystitis Manifest Itself?
Cervical Cancer: The Importance Of Prevention
Vulvodynia: What Are The Symptoms And How To Treat It
What Is Vulvodynia? Symptoms, Diagnosis And Treatment: Talk To The Expert
Accumulation Of Fluid In The Peritoneal Cavity: Possible Causes And Symptoms Of Ascites
What’s Causing Your Abdominal Pain And How To Treat It
Pelvic Varicocele: What It Is And How To Recognise The Symptoms
Can Endometriosis Cause Infertility?
Transvaginal Ultrasound: How It Works And Why It Is Important
Candida Albicans And Other Forms Of Vaginitis: Symptoms, Causes And Treatment
What Is Vulvovaginitis? Symptoms, Diagnosis And Treatment
Urinary Tract Infections: Symptoms And Diagnosis Of Cystitis
Cervical Cancer Screening, THINPrep And Pap Test: What Is The Difference?
Diagnostic And Operative Hysteroscopy: When Is It Necessary?
Techniques And Instruments For Performing Hysteroscopy
The Use Of Outpatient Hysteroscopy For Early Diagnosis
Utero-Vaginal Prolapse: What Is The Indicated Treatment?
Pelvic Floor Dysfunction: What It Is And How To Treat It
Pelvic Floor Dysfunction: Risk Factors
Salpingitis: Causes And Complications Of This Fallopian Tube Inflammation
Hysterosalpingography: Preparation And Usefulness Of The Examination
Gynaecological Cancers: What To Know To Prevent Them
Infections Of The Bladder Mucosa: Cystitis
Colposcopy: The Test Of The Vagina And Cervix
Colposcopy: What It Is And What It Is For
Vaginal Candida: Symptoms, Cause And Treatment


