Glaucoma: what it is and why it occurs
Glaucoma – also known as “the silent thief of sight” – is a chronic disease that affects the optic nerve
It can lead, if left untreated, to particularly negative consequences such as partial or total loss of vision.
Increased intraocular pressure (IOP) is the main risk factor and the only one currently treatable in almost all cases, especially in the primary forms.
Elevated IOP causes compression and distortion of the posterior ocular structures, particularly the scleral cribrosa plate which contains the optic nerve axons exiting the eyeball.
When there is actual damage to the optic nerve, the visual field begins to decrease starting from the most peripheral portions, proceeding gradually and involving more and more central portions of the visual field until complete loss of vision.
Glaucoma: why it occurs
Inside the eyeball there is a continuous flow of production and reabsorption of an aqueous liquid, which takes the name of aqueous humour, which has an optical function, linked to its transparency, static as it keeps the bulb tonic, nourishing as it it supplies glucose and oxygen and other nutrients to the cornea, to the lens, dynamic as it avoids the formation of adhesions between the structures of the eye and protects against trauma and photochromatic damage.
The outflow of aqueous humor occurs at the trabecular meshwork which, due to a reduction in its functions, can slow down the reabsorption of the aqueous humor produced, causing an increase in intraocular pressure.
The increase in pressure inside the eye, caused by a stagnation of unabsorbed fluid, can cause substantial damage to the optic nerve and, consequently, the development of glaucoma.
Glaucoma: symptoms
As anticipated, glaucoma is also known as “the silent thief of sight” as, in its initial stage, it does not present any symptoms detectable by the patient.
Only from the moment in which the optic nerve begins to be damaged due to the high intraocular pressure – which normally should not exceed 10 – 20 mmHg (millimeters of mercury) – the person suffering from glaucoma will begin to show the first symptoms of the disease: the loss of portions of the visual field.
The loss of portions of the visual field occurs progressively.
The first portion of the visual field that glaucoma will take away from the affected subject is the lateral, superior and inferior one.
Initially the latter may not notice a narrowing of his field of vision.
Glaucoma, unfortunately, is not a linearly advancing disease.
This means that, if these alarm bells are ignored and an ophthalmological examination is not promptly carried out which will diagnose the disease and then treat it, glaucoma could also subtract the central portion of the visual field of the subject, who would be in a state of permanent blindness.
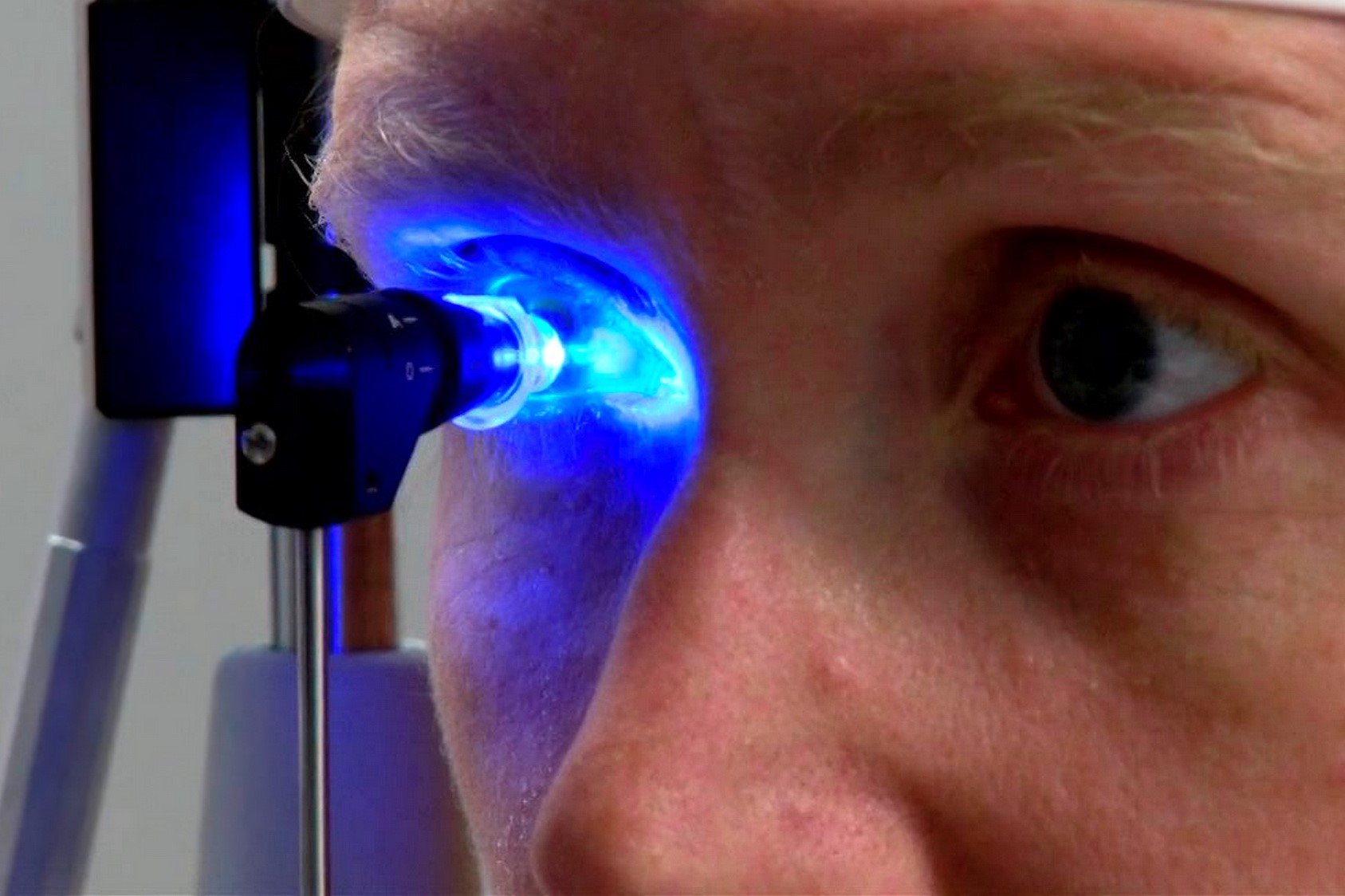
Glaucoma: the diagnosis
The specialist visit assumes fundamental importance since the initial stages of the pathology are not characterized by particularly evident symptoms.
During the visit it will therefore be possible to carry out a tonometry to verify the alteration of the intraocular pressure, and a gonioscopy which allows to visualize the structures responsible for the outflow and production of the aqueous humor and thus proceed to the distinction of the various types of glaucoma.
In addition, pachymetry may be needed to measure the thickness of the cornea.
Fundamental for the diagnosis and to evaluate the progression of the disease are:
- Perimetry or examination of the visual field or the evaluation of the extension of the visual field
- An OCT (optical coherence tomography) to check the thickness of the nerve fibers that surround the optic nerve.
In other cases you can also use:
- A computerized FDT (Frequency Doubling Technology) perimetry to detect visual field deficits or alterations
- Evaluation test for the perception of colors and contrasts
- A fluorescein angiography (FA) to highlight the possible presence of retinal ischemic areas in the presence of a type of glaucoma defined as neovascular, secondary to systemic or ocular pathologies
Glaucoma: three different types
Once all the specific tests requested by the ophthalmologist have been carried out, it will be easier for the specialist to provide a precise diagnosis to the patient.
If this confirms the presence of glaucoma, a first important subdivision will be between open angle glaucoma, narrow angle glaucoma and congenital glaucoma.
Open angle glaucoma
If the diagnosis confirms the presence of an open angle glaucoma, the course of the disease will be slow and progressive, caused by the alteration of the pressure of the aqueous humor inside the eye.
This type of glaucoma will slowly degenerate causing no symptoms other than the progressive reduction of the visual field
Narrow angle glaucoma
If, on the other hand, the diagnosis confirms the presence of narrow-angle glaucoma – fortunately less widespread disease – the glaucoma will degenerate rather quickly.
In fact, the disease can occur suddenly, caused by an abrupt interruption of the reabsorption of the aqueous humor at the trabecular meshwork.
This abrupt obstruction configuring a picture of so-called “acute glaucoma” will be immediately perceived by the patient, triggering eye pain, nausea, vomiting, blurry vision and halos around light sources.
Treatment must also be timely to avoid irreversible sequelae to visual function.
Congenital glaucoma
This form of glaucoma can manifest itself from birth or in the very first years of the child’s life.
It is due to a malformation of the outflow tracts of the aqueous humor and is among the leading causes of childhood blindness.
Glaucoma: how to cure it
In an initial phase, glaucoma – especially in its open angle version – can be treated with drug therapy based on eye drops.
If this treatment proves insufficient to control the disease and the ocular pressure continues its slow damage to the optic nerve, parasurgical intervention (use of lasers) or surgery is generally used.
Surgical and parasurgical interventions are all aimed at obtaining control of ocular pressure where medical therapy has proved ineffective.
Furthermore, they are many and not all of them are indicated for the different types of glaucoma.
In open angle glaucoma, more or less invasive techniques are often used which have the aim of restoring the outflow paths of the aqueous humor or creating new ones, or of reducing the production of aqueous humor, acting on the structures that release it, obtaining in each case a decrease in intraocular pressure.
The main ones are:
- Laser Trabeculoplasty (ALT or SLT)
- Cyclodestructive procedures (e.g. cyclophotocoagulation, cyclocryotherapy)
- Penetrating filtering surgery (trabeculectomy)
- Non-perforating filtering surgery (e.g. canaloplasty)
- Shunt procedures (microinvasive anterior drainage techniques, posterior drainage devices)
- In the treatment of narrow angle glaucoma are also useful:
- YAG laser iridotomy
Cataract surgery
Depending on the type of glaucoma diagnosed, the specialist doctor will reserve the right to direct the patient towards the treatment that best suits his needs.
Glaucoma: how to prevent its occurrence
There is no real way to prevent the occurrence of glaucoma.
However, there are some subjects at risk, who – for prevention – are strongly advised to undergo periodic eye examinations so as to detect any onset of the disease in time.
Patients who have relatives with glaucoma, who have a percentage chance of developing the disease themselves between 10 and 15%
- Subjects with reduced thickness of the cornea
- Subjects who have an optic disc that appears altered and does not present in its normal anatomy
- Subjects complaining of visual field amplitude defects
- Patients with ocular defects attributable to the possible appearance of glaucoma
- Those with high myopia
- Diabetic subjects
Subjects who – due to other pathologies – are forced for a long time to administer cortisone drugs which could cause an increase in ocular tone
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Glaucoma: What Is True And What Is False?
Eye Health: Prevent Conjunctivitis, Blepharitis, Chalazions And Allergies With Eye Wipes
What Is Ocular Tonometry And When Should It Be Done?
Dry Eye Syndrome: How To Protect Your Eyes From PC Exposure
Autoimmune Diseases: The Sand In The Eyes Of Sjögren’s Syndrome
Dry Eye Syndrome: Symptoms, Causes And Remedies
How To Prevent Dry Eyes During Winter: Tips
Blepharitis: The Inflammation Of The Eyelids
Blepharitis: What Is It And What Are The Most Common Symptoms?
Stye, An Eye Inflammation That Affects Young And Old Alike
Diplopia: Forms, Causes And Treatment
Exophthalmos: Definition, Symptoms, Causes And Treatment
Eye Diseases, What Is Entropion
Hemianopsia: What It Is, Disease, Symptoms, Treatment
Diseases Of The Ocular Conjunctiva: What Are Pinguecula And Pterygium And How To Treat Them
What Is Ocular Pterygium And When Surgery Is Necessary
Vitreous Detachment: What It Is, What Consequences It Has
Macular Degeneration: What It Is, Symptoms, Causes, Treatment
Conjunctivitis: What It Is, Symptoms And Treatment
How To Cure Allergic Conjunctivitis And Reduce Clinical Signs: The Tacrolimus Study
Bacterial Conjunctivitis: How To Manage This Very Contagious Disease
Allergic Conjunctivitis: An Overview Of This Eye Infection
Keratoconjunctivitis: Symptoms, Diagnosis And Treatment Of This Inflammation Of The Eye


