Haemorrhoids: the newest tests and treatments to treat them
Haemorrhoids are a much more frequent problem than one might think. According to studies, it is estimated that as much as 10% of the world’s adult population is affected, and the incidence is prevalent among those over 50 years of age
Only a tiny fraction, however, talk to their doctor about it: it is an annoying ailment, but often a taboo subject.
Yet the first step to solving it is to understand it correctly, also with the help of a specific examination, the anoscopy.
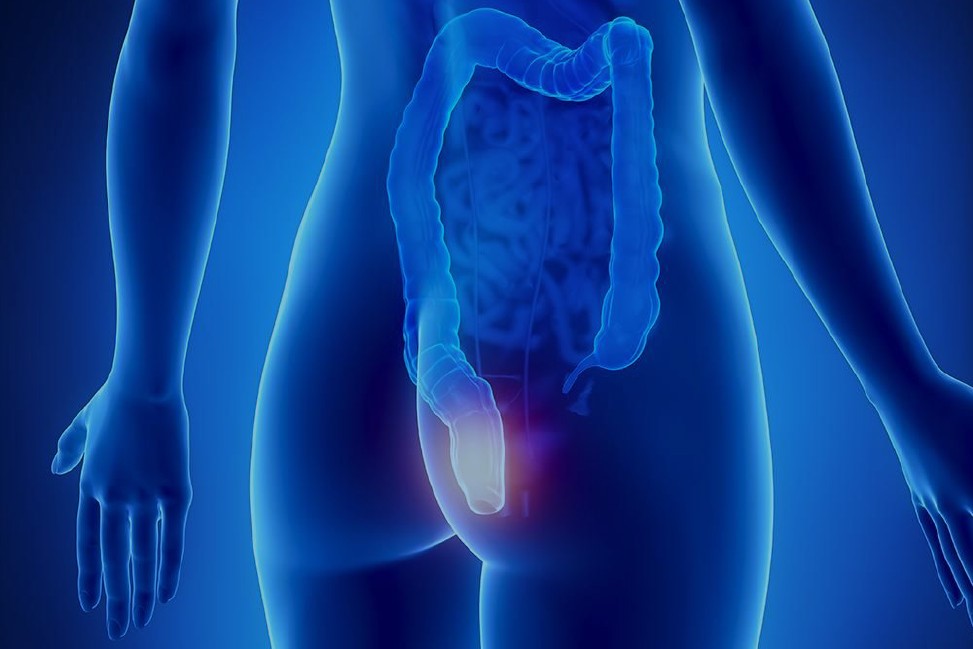
What are haemorrhoids
The haemorrhoids, or rather the haemorrhoid plexuses, are one of the components of the anal canal, whose task is to allow and encourage evacuation and adequate continence of faeces and gas.
In detail, they are small, highly vascularised pads of tissue that are absolutely physiological.
However, under certain conditions, they can become a problem with a considerable impact on the quality of life of men and women.
Haemorrhoids evolve from physiological to pathological when they become inflamed, swell, and leak from their seat (haemorrhoidal prolapse).
Causes and risk factors of haemorrhoids
The most frequent cause of inflammation and leakage of haemorrhoids is a combination of predisposition associated with a ‘bad’ lifestyle.
Among the factors that contribute most to haemorrhoid prolapse are:
- sedentariness;
- obesity;
- low-fibre diet;
- spending too much time on the toilet, reading magazines or looking at a mobile phone.
To these causes must be added the ‘factor’ pregnancy which, although physiological, can contribute to the development of haemorrhoidal pathology due to the increasing weight of the uterus on the pelvis.
How haemorrhoids manifest themselves
When haemorrhoids become enlarged, they cause:
- swelling sensation;
- itching;
- more or less significant bleeding.
The role of the proctologist
When these symptoms occur, it becomes essential to consult a proctology specialist.
First of all, it is necessary to make a correct diagnosis, since there are many pathologies that affect the anal canal and consequently may mimic or be associated with haemorrhoids:
- fissures;
- abscesses;
- obstructed defecation syndrome;
- pelvic floor dysfunction;
- certain tumours and chronic inflammatory bowel disease.
Haemorrhoids themselves, then, can present with different levels of severity: from grade 1 to grade 4
In addition, it is essential that the treatment of haemorrhoid pathology must be personalised for each individual patient.
The weapons available to cure haemorrhoid pathology are diverse and must be filtered and selected, without embarrassment, in agreement with the patient on the basis of
- eating habits;
- how defecation occurs;
- sexual habits and attitudes.
The proctologist should proceed to:
- a detailed personal, dietary anamnesis on evacuation habits;
- a precise and thorough examination of the anal and perianal region;
- an anoscopy.
The examination for haemorrhoids: the anoscopy
The anoscopy examination consists of the introduction into the anus, after application of an anaesthetic lubricant to minimise discomfort, of a cylindrical instrument made of transparent plastic about 6 centimetres long by 2 centimetres in diameter, connected to a light source or a high-resolution camera.
Thanks to the presence of the camera, which in turn is connected to the computer screen, the proctologist is able to observe the inside of the anal canal directly and in detail, thus being able to clarify the diagnosis and also rule out the presence of any neoplasm in the last part of the anal canal.
How to prepare for anoscopy
The examination requires prior cleansing, which is generally achieved with
- an evacuative enema the evening before;
- an enema 2-3 hours before the examination.
Therapy: personalised and multidisciplinary
Healing from haemorrhoids is possible through a shared pathway between proctologist and patient.
When necessary, a multidisciplinary team consisting of radiologist, endoscopist, physiotherapist and nutritionist is also involved, who must necessarily focus on the needs and expectations of the individual patient.
Surgery? Not always necessary
Before resorting to surgery, in most cases, a common path is shared with the patient, ranging from improving evacuation dynamics to modifying, if necessary, diet, fibre intake and the use of specific medicines, which differ from patient to patient with the application or not of creams and ointments locally.
If surgical treatment is necessary, the specialist may use very different techniques, depending on the case:
(a) outpatient procedures, such as:
- elastic ligation of haemorrhoids;
- infrared photocoagulation;
- sclerosants,
- interventions such as laser therapy or embolisation, whereby certain arteries supplying the haemorrhoid venous plexuses are closed;
b) surgical interventions, such as:
- haemorrhoidopexy, a technique that corrects and repositions excess tissue without removing the haemorrhoids;
- transanal dearterisation, i.e. ligation of the haemorrhoidal arteries;
- haemorrhoidectomy, i.e. removal of the haemorrhoids.
We can say that the possible treatments for treating haemorrhoids are many and varied: the important thing is to find an ad hoc solution for each individual patient and to guarantee the best possible result.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Raising The Bar For Pediatric Trauma Care: Analysis And Solutions In The US
Pinworms Infestation: How To Treat A Paediatric Patient With Enterobiasis (Oxyuriasis)
Intestinal Infections: How Is Dientamoeba Fragilis Infection Contracted?
Gastrointestinal Disorders Caused By NSAIDs: What They Are, What Problems They Cause
Intestinal Virus: What To Eat And How To Treat Gastroenteritis
What Is Proctalgia Fugax? Symptoms, Causes And Treatment
Internal And External Haemorrhoids: Causes, Symptoms And Remedies


