Helicobacter Pylori infection: new therapeutic horizons
Rapid diagnosis and eradication of Helicobacter Pylori enables prevention and treatment of major gastric diseases
Helicobacter Pylori, characteristics and epidemiology
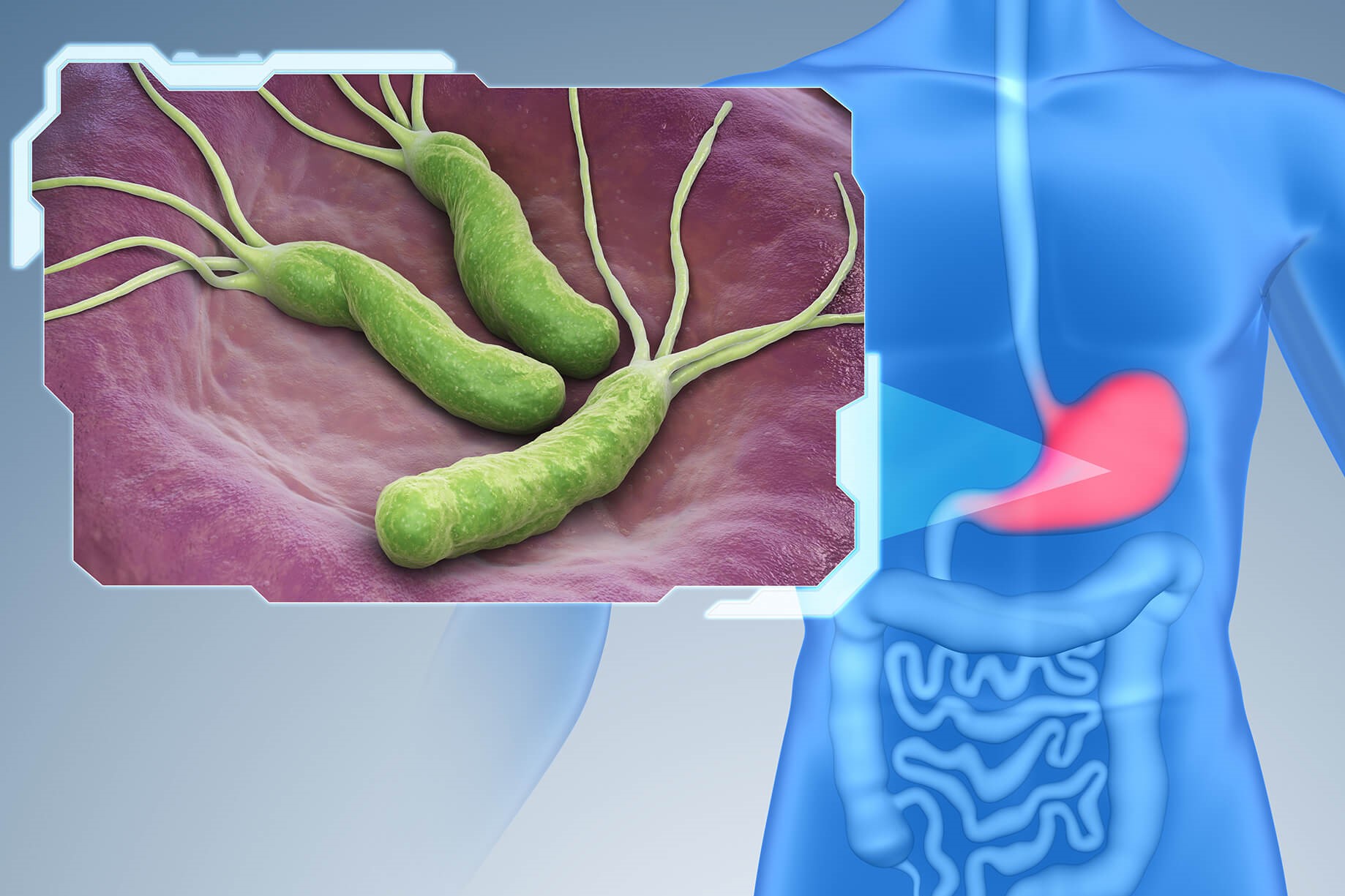
Helicobacter Pylori is a flagellated, acid-tolerant, gram-negative bacterium whose ideal habitat is the gastric mucus in the human stomach.
Its resistance to acidic pH values between 1 and 2 is conferred by the production of the enzyme urease, which creates a microenvironment around the bacterium that is compatible with its existence.
Numerous studies in the medical literature have demonstrated the pathogenic role of this microorganism as a co-factor in numerous diseases: gastritis, duodenitis, gastric ulcer, duodenal ulcer, MALT-lymphoma and gastric cancer.
Most individuals are asymptomatic carriers: the presence of an efficient immune system ensures adequate protection, whereas individuals with immunodeficiency conditions are particularly susceptible to this type of infection.
The most likely mode of transmission is considered to be the faeco-oral route.
Other possible routes of contagion are contact with contaminated water or endoscopic instruments, but there are as yet no definitive data on this.
Methods for diagnosing Helicobacter Pylori
The methods can be divided into invasive (oesophagogastroduodenoscopy and biopsies) and non-invasive (respiratory test, faecal antigen search, blood antibody search).
In the last 10 years, the most widely used test has undoubtedly been the Urea Breath Test (UBT), which consists of having the patient ingest a drink containing urea labelled with a carbon isotope and then assessing the presence of labelled carbon dioxide in the exhaled air.
The test is performed on an outpatient basis, is relatively low cost and has high sensitivity and specificity.
Even in the presence of highly reliable non-invasive methods such as the Urea Breath Test, the upper endoscopic examination (oesophagogastroduodenoscopy) continues to play a central role in the diagnostic-clinical pathway related to Helicobacter Pylori infection, mainly in subjects over 45 years of age, as it allows a direct assessment of any lesions or conditions associated with this infection (gastritis, duodenitis, gastric ulcer, duodenal ulcer, etc.).
Classical therapies and new therapeutic horizons
As mentioned above, Helicobacter Pylori is the cause of various diseases (gastric and extra-gastric) and for this reason, when the infection is diagnosed, it should be eradicated regardless of the presence of symptoms or any complications.
The eradication of Helicobacter Pylori has become considerably more difficult in recent decades due to the increased prevalence of bacterial strains resistant to antibiotics, particularly clarithromycin.
The most recent guidelines have stipulated that Helicobacter Pylori patients should only be treated first-line with classical therapy (proton pump inhibitor combined with amoxicillin and clarithromycin) or alternative schemes (sequential or concomitant therapy) in countries with a low prevalence of clarithromycin-resistant strains (<15%).
Also, in countries with a high prevalence of clarithromycin-resistant strains (>15%), including Italy, the first line of therapy should be quadruple therapy (proton pump inhibitor combined with bismuth subcitrate, tetracycline and metronidazole).
A new ‘3-in-1’ formulation containing bismuth subcitrate, tetracycline and metronidazole (Pylera, Allergan – Dublin, Ireland) has recently been introduced on the market. Several recent studies have demonstrated a high efficacy of this new formulation, in combination with a proton pump inhibitor, both as first-line therapy and as ‘rescue therapy’ after a failed therapeutic attempt with other lines of treatment.
A recent Italian, retrospective, multicentre study, coordinated by Professor Zagari showed high eradication rates (91.4% as first-line therapy and 89.4% as second-line), overlapping between Northern and Southern Italy.
Adverse events (most frequent: nausea, vomiting and diarrhoea) during treatment with quadruple therapy (Pylera) were reported in about 30% of patients but only in 6% were classified as severe and caused discontinuation of the treatment regimen.
Total treatment compliance was 94.9%.
In conclusion, we can state that the new “3-in-1” formulation of quadruple therapy (Pylera) has proven to be highly effective and well tolerated both as first-line therapy and as “rescue therapy” in case of failure of other therapies.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Helicobacter Pylori: How To Recognise And Treat It
Irritable Bowel Syndrome (IBS): A Benign Condition To Keep Under Control
Gastroesophageal Reflux: Causes, Symptoms, Tests For Diagnosis And Treatment
Ulcerative Colitis: Phase III Study Shows Efficacy Of Investigational Drug Ozanimod
Peptic Ulcer, Often Caused By Helicobacter Pylori
Helicobacter Pylori Infection: What Causes It, How To Recognise It And Treatment
Helicobacter Pylori Infection: What Are The Symptoms?


