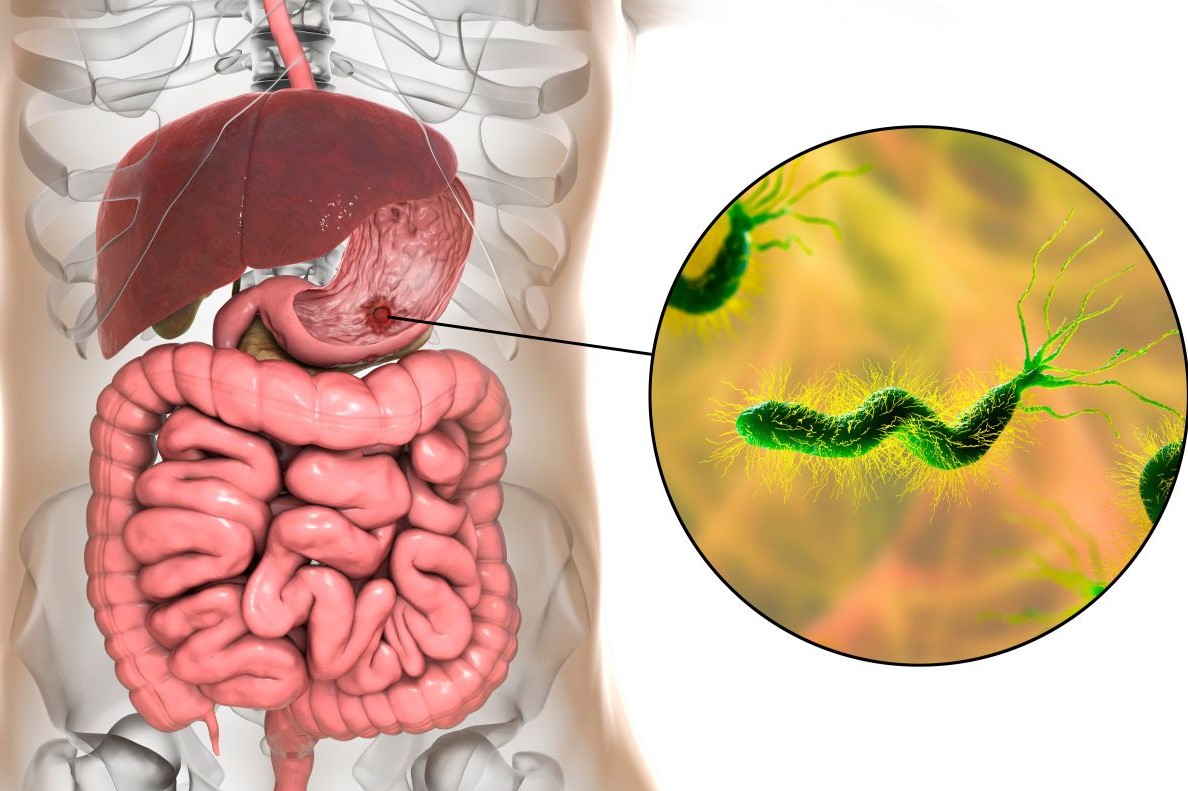
Helicobacter Pylori: the guidelines
Helicobacter pylori infection is now well known, as are its consequences and the benefits of eradication, since it was first identified in the early 1980s
Compared to previous indications, new guidelines have been published in late 2021 that partially modify the known indications, so here are the most significant aspects that have emerged from recent research:
- Infection with the Helicobacter Pylori bacteria continues to be a major health problem worldwide with significant mortality and morbidity due to peptic ulcer and gastric cancer.
- The most significant factor in reducing infection and transmission appears to be improvements in the socio-economic status of populations and individuals that allow greater access to treatment and more appropriate use of resources.
- Uncertainties still exist as to the route of transmission, which seems particularly frequent between family members, especially via the oro-oral or gastro-oral route, while orofecal transmission is less likely and still undefined via water, food, pets or insects.
- Approximately 50% of the world’s population is infected, with wide geographical variations, and the major determinant of the prevalence of infection appears to be socio-economic status in childhood, which determines the level of hygiene, care and health education. Prevalence increases with age.
- The relationship between infection, ulcer and neoplasia is confirmed although atrophy and metaplasia are irreversible and require endoscopic surveillance.
- Most infected patients are asymptomatic and only in one third of infected patients with functional dyspepsia do symptoms disappear after eradication.
- The indication to treat all positive patients even in the absence of symptoms or associated pathology is confirmed and the diagnostic modalities, first and foremost the mucosal biopsy during gastroscopy as well as the breath test to confirm eradication, are confirmed.
Helicobacter pylori eradication therapy
Finally, a few considerations regarding therapy for Helicobacter pylori eradication.
Which antibiotics should be used for eradication?
The determining factor for successful therapy is known drug resistance to previous antibiotic therapy.
Pharmacoresistance has great geographical variability, determined mainly by the use and misuse of antibiotics in the population and in the individual subjects to be treated, particularly clarithromycin.
Treatment choices must take into account the epidemiological situation of resistance in different geographical areas.
Since the issuance of the previous guidelines, increased resistance to clarithromycin had already emerged, so the classic triple therapy (clarithromycin, amoxicillin and proton pump inhibitor) should no longer be used in areas where resistance to clarithromycin is higher than 15%, i.e. in most of Europe and the USA.
Secondary resistance after therapy is common (especially with metronidazole clarithromycin and levofloxacin), so repeating the same therapy has low chances of success and should be avoided.
Dose and duration of therapy influence the probability of eradication as well as compliance and smoking.
The standard of care is quadruple therapy with the addition of metronidazole or alternatively a schedule using bismuth and tetracyclines combined with pump inhibitor and metronidazole.
The use of levofloxacin in a triple combination scheme is a good option, but not recommended as a first choice.
Helicobacter Pylori, duration of therapy
Therapy lasts 14 days and, in the case of rescue therapy after resistant infections, it is advisable to avoid the antibiotics already used and to consider schemes containing bismuth and levofloxacin.
It is not recommended to use blood tests that are likely to remain indefinitely positive to diagnose a persistent infection.
Indications for gastroscopy
Up to the age of 60 with no warning symptoms, it may be indicated to treat positive helicobacter pylori dyspepsia with eradication without endoscopy and, even in the presence of iron deficiency, it may make sense to check for infection.
How can Helicobacter Pylori eradication be verified?
Eradication must be verified no sooner than 4 weeks after the end of therapy, using a breath test or faecal antigen and after discontinuing bismuth and antibiotics for at least 28 days and proton pump inhibitors for at least 14 days.
Finally, before starting treatment with non-steroidal anti-inflammatory drugs, eradication of Helicobacter pylori reduces the incidence of ulcers and complications associated with bleeding.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Helicobacter Pylori: How To Recognise And Treat It
Irritable Bowel Syndrome (IBS): A Benign Condition To Keep Under Control
Gastroesophageal Reflux: Causes, Symptoms, Tests For Diagnosis And Treatment
Ulcerative Colitis: Phase III Study Shows Efficacy Of Investigational Drug Ozanimod
Peptic Ulcer, Often Caused By Helicobacter Pylori
Helicobacter Pylori Infection: What Causes It, How To Recognise It And Treatment
Helicobacter Pylori Infection: What Are The Symptoms?
Helicobacter Pylori Infection: New Therapeutic Horizons


