Hydrocephalus: causes, treatment, consequences, life expectancy
In medicine, ‘hydrocephalus’ refers to a condition in which there is an accumulation of cephalorhachid fluid (also called ‘CSF’) at the level of the cerebral ventricles that dilate
The consequence of the abnormal presence of this fluid in an inextensible compartment such as the adult skull is an increase in the pressure inside it (intracranial hypertension), which compresses the brain and prevents the incoming blood from the heart from efficiently supplying the brain tissue.
Hydrocephalus is thus the chronic presence of excess cephalorachid fluid
If hydrocephalus develops instead in a newborn, in an infant or in any case before the physiological sealing of the cranial sutures, a picture of macrocephaly will be present, since the skull in the first months of life is expandable, unlike that of the adult.
Hydrocephalus is not a pathology per se, but the manifestation of another underlying brain problem
Therefore, the treatment and prognosis of a hydrocephalic adult or child depends not only on the hydrocephalus itself, but also on the underlying cause.
Why does CSF accumulate?
Under normal conditions, CSF is very similar to the liquid part of the blood and contains sugars and various mineral salts.
It is produced by special structures called choroid plexuses (particularly in the lateral, but also in the 3rd and 4th ventricles), has its own circulation through the ventricles and on the surface of the brain and spinal cord, and is finally reabsorbed by certain veins contained on the surface of the brain, which make it flow into the blood circulation.
Normal CSF values range from 150 to 200 ml.
The daily production of CSF is about 350 to 450 ml of fluid per day, ensuring an abundant but balanced turnover under normal conditions.
Its main purpose is to maintain the brain and spinal cord in a protective environment and its quantity in the cerebral ventricles must be kept constant at all times.
As already mentioned, hydrocephalus is caused by the presence of an abnormal accumulation of cerebral spinal fluid (CSF) within the cavities of the cerebral ventricles.
CSF accumulates basically for three reasons
- because there is an overproduction of it at the level of the choroid plexuses;
- because it finds an obstacle to its physiological circulation;
- because there is an alteration in the mechanism of its reabsorption.
Based on this distinction, three types of hydrocephalus are classified:
- hypersecretory hydrocephalus (from CSF overproduction): more frequent in children, caused by carcinomas or papillomas of the choroid plexuses;
- obstructive hydrocephalus (from obstruction of CSF circulation): often caused by malformations or other pathologies leading to obstruction, such as tumours and cerebral haemorrhage;
- obstructive or non-communicating hydrocephalus (from reduced reabsorption): mainly caused by haemorrhage or infectious processes.
Difference between communicating and non-communicating hydrocephalus
Depending on where the accumulation of cephalic spinal fluid occurs, two forms of hydrocephalus are classified
- communicating (non-obstructive) hydrocephalus: CSF accumulates in the cerebral ventricles and subarachnoid space.
- non-communicating (obstructive) hydrocephalus: CSF accumulates exclusively within the ventricular cavities and NOT in the subarachnoid space.
Normotensive hydrocephalus
Normotensive hydrocephalus is a special type of communicating (non-obstructive) hydrocephalus, in which the increase in intracranial pressure, due to the accumulation of CSF, becomes stable, i.e. the formation of excess cerebrospinal fluid is balanced by an increase in absorption: the intracranial pressure gradually decreases, but still remains at a slightly higher level than normal.
Due to this equilibrium, the patient does not show the classic symptoms of intracranial hypertension such as headache, nausea, vomiting or unconsciousness, but instead displays a classic symptom triad consisting of:
- difficult gait;
- urinary incontinence;
- mental deterioration.
Precisely because of these symptoms, normalised hydrocephalus is often confused with Parkinson’s or Alzheimer’s disease, due to its nature as a chronic pathology and initial symptoms.
Although the exact mechanism is unknown, normotensive hydrocephalus is thought to be a form of communicating hydrocephalus with altered reabsorption of cerebrospinal fluid in the granulations of the Pacchioni.
It may present as idiopathic hydrocephalus (i.e. a hydrocephalus whose underlying cause is unclear to physicians).
Causes of hydrocephalus in newborns and infants
The most common causes of hydrocephalus in newborns and infants are:
- infections contracted in utero (TORCH, cytomegalovirus, mysterious etc.) or in the perinatal period (bacterial meningitis)
- congenital malformations (stenosis of Silvio’s aqueduct, spina bifida, Chiari malformation, Dandy Walker syndrome, arachnoid or ventricular cysts);
- germinal matrix haemorrhages in the premature (intraventricular).
Causes of hydrocephalus in adults and young people
The most common causes of hydrocephalus in young people and adults are:
- cerebral neoplasms obstructing the CSF circulation;
- arachnoid cysts;
- haemorrhages that create direct obstruction of the CSF circulation or indirect obstruction through increased hypertension in the skull, which in turn prevents proper CSF circulation.
Haemorrhage typically occurs due to trauma (e.g. car accident or sports injury), haemorrhagic cerebral stroke and ruptured cerebral aneurysm.
Symptoms of hydrocephalus
Whatever the cause, the signs and symptoms are peculiar and differ depending on the age at which the problem occurs.
In the newborn there is an abnormal increase in head circumference (macrocrania), with prominence and tension of the anterior fontanel, congestion of the epicranial venous reticulum, lethargy or irritability.
In the child after the age of one year, in whom fusion of the cranial sutures has occurred, appear instead
- repeated vomiting;
- headache;
- tendency to drowsiness;
- visual disturbances;
- sometimes epileptic seizures.
Similar symptoms, sometimes associated with narcolepsy, are also found in young people and adults.
Diagnosis of hydrocephalus in adults
Diagnosis in adults is based on:
- clinical evaluation of symptoms;
- lumbar puncture (spinal tap) is usually the first step for diagnosis, as it allows the endocranial pressure to be measured: in most cases it exceeds 155 mmH2O. This diagnostic procedure consists of taking a CSF sample using a needle inserted between the L3-L4 or L4-L5 vertebrae.
Clinical improvement after CSF removal (30 ml or more) has a high predictive value for the success of subsequent brain shunt implantation;
- infusion testing;
- neuropsychological testing;
- external lumbar drainage;
- CT scan: may show enlarged brain ventricles without convolutional atrophy;
- magnetic resonance imaging: may show some degree of trans ependymal migration of CSF surrounding the ventricles;
- arteriography: sometimes used to ascertain suspected hydrocephalus. It consists of the radiological study of the morphology of arteries, carried out by injecting – into the same artery to be analysed – a contrast liquid.
Diagnosis of hydrocephalus in newborns and infants
Diagnostic examinations are already possible during pregnancy (morphological ultrasound).
After birth, in addition to the clinic, the doctor is aided in the diagnosis by transfontanellar brain ultrasound and magnetic resonance imaging of the brain, which also makes it possible to ascertain the concomitant presence of underlying brain lesions.
How is hydrocephalus treated?
Hydrocephalus is generally treatable successfully, while the underlying cause may be treated in some cases or not treated in others, depending on the type.
In addition, both hydrocephalus and the underlying cause may or may not have irreversibly damaged brain tissue.
The treatment of hydrocephalus strongly depends on a few factors:
- triggering cause;
- clinical course;
- severity;
- symptoms it causes;
- age of the patient;
- possible presence of other pathologies;
- evaluation of the risks and benefits associated with the surgical procedure.
In cases of obstructive hydrocephalus due to a lesion obstructing the CSF circulation, surgical treatment of the lesion (removal of the neoplasm, arachnoid cyst, etc.) resolves the hydrocephalic problem in almost all cases.
Current surgical treatment involves two options
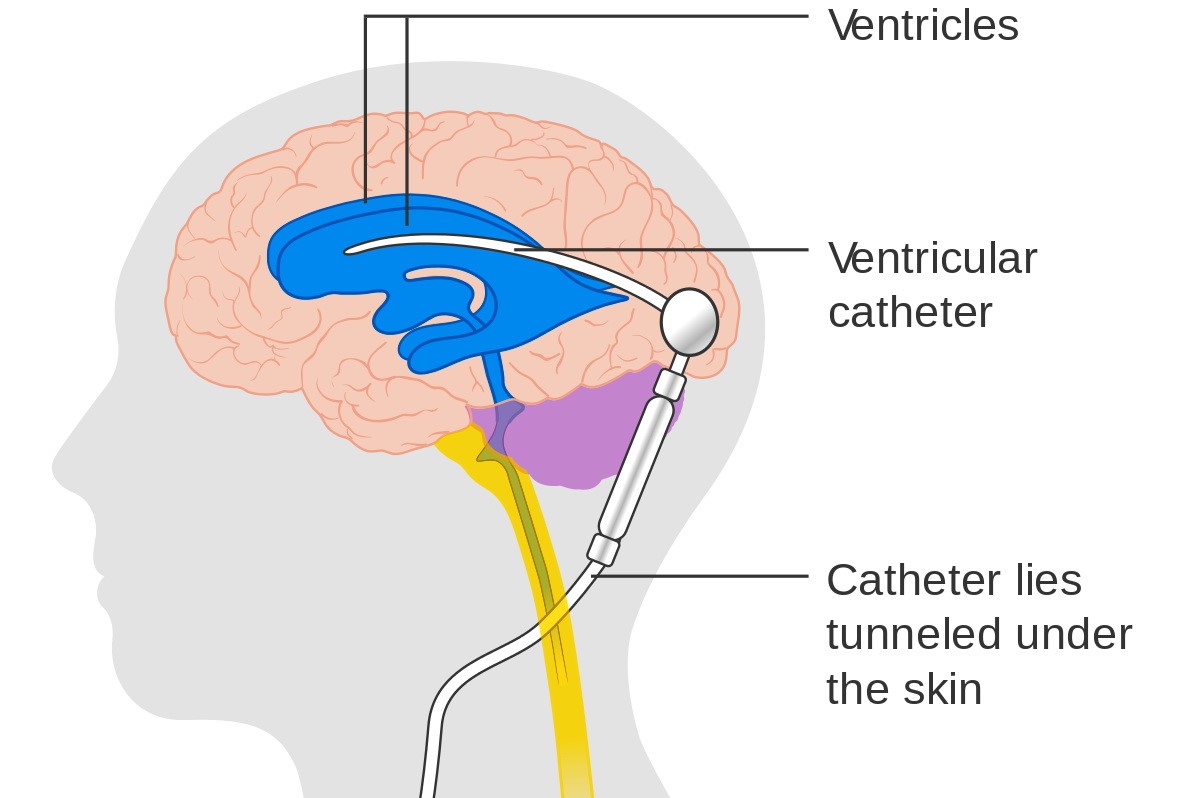
- implantation of ventriculo-peritoneal liquid shunts;
- use of endoscopic techniques (ventricle-cystostomy).
In children with hydrocephalus without obvious CSF reabsorption problems (stenosis of Silvio’s aqueduct, intraventricular arachnoid cysts), it is possible with the use of the endoscope, a fibre-optic instrument, to create in direct vision a communication between the floor of the third ventricle and the CSF cisterns of the skull base, through which an alternative pathway to obstructing the CSF circulation can be generated.
The technique involves a single cranial incision in the right frontal region of approximately 2 cm.
Risks of surgery and prognosis
In 1-2% of cases, bleeding within the ventricle may occur, which may require the placement of a temporary external CSF drain; other times, failure of the ostomy may occur (15-25% of cases), which can be resolved with a second endoscopic attempt or with the implantation of a ventricle-peritoneal shunt system.
For both surgical techniques the average hospital stay after the operation is 4-6 days; after 7-10 days the stitches are removed.
The prognosis is generally very good.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Obstructive Sleep Apnoea: What It Is And How To Treat It
Obstructive Sleep Apnoea: Symptoms And Treatment For Obstructive Sleep Apnoea
Our respiratory system: a virtual tour inside our body
Tracheostomy during intubation in COVID-19 patients: a survey on current clinical practice
FDA approves Recarbio to treat hospital-acquired and ventilator-associated bacterial pneumonia
Hydrothorax: Causes, Pathologies, Symptoms, Diagnosis And Treatment


