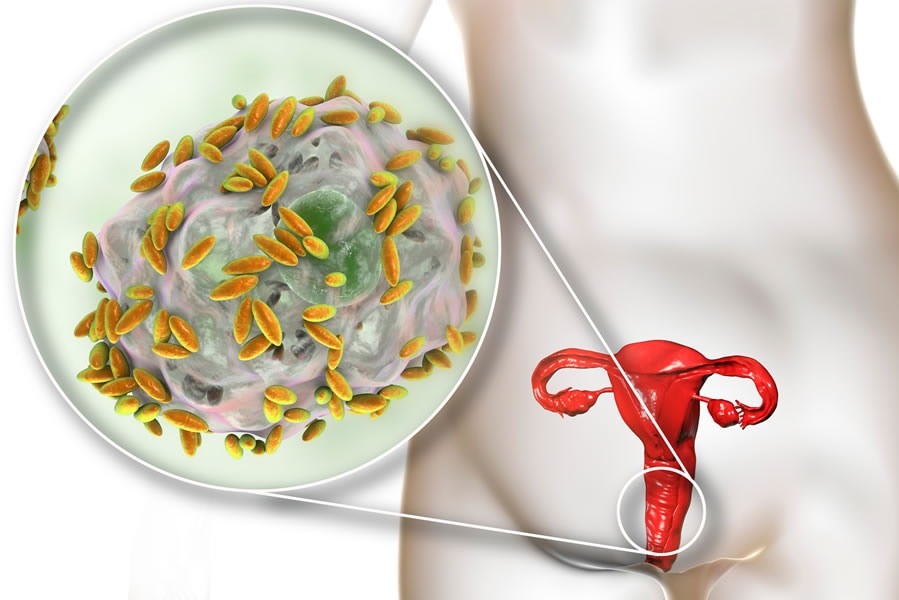
Inflammations of the genital apparatus: vaginitis
Vaginitis is the inflammation of the vagina. It may manifest as white or yellowish discharge, sometimes smelly, and may involve itching and burning
It is favoured by changes in the vaginal pH, which reduce the physiological balance of bacteria normally present in the vagina, favouring the entry of pathogenic germs.
Vaginitis can be caused by bacteria (Gardnerella), fungi (Candida) and protozoa (Trichomonas), but it can also be triggered by hormonal changes (such as reduced oestrogen levels in the post-menopausal period).
What is vaginitis?
The most common causes are:
- bacteria
- fungi
- parasites
- use of irritating products
- hormonal changes
What are the causes of vaginitis?
There can be several causes of vaginitis.
One can therefore distinguish:
- Bacterial vaginitis: generally the ‘good’ bacteria present in the vagina outnumber the ‘bad’ bacteria. It can happen, however, that the ‘bad’ bacteria increase in number excessively, upsetting the balance of the vaginal bacterial flora and causing bacterial vaginitis.
- Fungal vaginitis: occurs when the vaginal balance undergoes changes (e.g. after antibiotic therapy) that allow specific fungi – usually candida albicans – to take root.
- Parasitic vaginitis: is typically caused by a protozoan called Trichomonas vaginalis. It is one of the most common sexual infections: the microorganism usually infects the urinary tract in men asymptomatically and is then transmitted to the woman through sexual intercourse.
- Non-infectious vaginitis: various products – intimate cleansers, washing machine detergents, tampons, tampons, vaginal sprays, douches, spermicidal products – can irritate the tissues of the vagina.
- Finally, ‘atrophic vaginitis’ is defined as inflammation of the vagina caused by hormonal changes (a rather frequent disorder after the menopause).
- Actinic vaginitis: is the inflammation of the vagina created by radiation therapies, carried out in the treatment of certain cancers.
What are the symptoms of vaginitis?
Symptoms may include:
- change in colour, smell and/or quantity of vaginal discharge
- itching and/or burning
- pain or irritation during sexual intercourse
- painful urination
- light bleeding
Certain symptoms can help distinguish the type of vaginitis:
- in the case of bacterial vaginitis, the main symptom is malodorous greyish-white discharge. The smell may be fishy and may be stronger after menstruation or sexual intercourse;
- in fungal vaginitis the main symptom is vulvar/vaginal itching, accompanied by white, thick secretions (similar to cottage cheese);
- in trichomoniasis vaginitis, the main symptom is discharge that may range from yellowish to greenish, and may be foamy. It is usually accompanied by vulvo-vaginal burning.
How to prevent vaginitis?
Prevention is important:
- Avoid vaginal irrigations if not necessary: the vagina requires normal cleansing, just like other parts of the body. Subjecting the vagina to too intense washing – such as vaginal irrigations – can upset the balance of bacteria normally present in it and increase the risk of infection.
- After using the toilet, it is a good idea to wipe from front to back, and not the other way around: this prevents the spread of faecal bacteria to the vagina.
- When washing, prefer a shower to a bath: rinse off the detergent used and dry thoroughly to avoid stagnating moisture. Do not use soaps that are too aggressive.
- Using a condom during sexual intercourse helps avoid vaginitis that is sexually transmitted.
Diagnosis
Sometimes it is the patient’s own reported symptoms that allow the specialist to make a diagnosis.
Obviously, a specialist gynaecological examination is very helpful.
If necessary, during the examination, the specialist can take a sample of secretions to be analysed in the laboratory to confirm the type of vaginitis.
Treatments
Given the multiplicity of causes of vaginitis, there are several treatments that patients can undergo.
In the case of bacterial vaginitis, antibiotics may be prescribed to be taken by mouth or applied locally (in the form of cream, ova or gel).
Treatment usually lasts 5-7 days.
Fungal vaginitis is generally treated with antifungal drugs.
They can be administered orally or locally (creams, ovules, tablets or vaginal capsules).
Oral antibiotics are generally prescribed against trichomoniasis vaginitis, but there are also specific topical treatments.
Atrophic vaginitis can be effectively treated with oestrogen in various forms (tablets, gels, creams, patches).
The use of oestrogens must always be evaluated by the specialist and avoided in the presence of contraindications.
Where it is not possible to prescribe hormone therapies, the use of emollient and lubricating products will be limited.
These same products are also mostly used in ray vaginitis.
To treat non-infectious vaginitis, it is necessary to identify – and remove – the source of irritation.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Cervical Dysplasia: What Are The Risk Factors And How To Treat It
Vulvodynia: What Are The Symptoms And How To Treat It
What Is Vulvodynia? Symptoms, Diagnosis And Treatment: Talk To The Expert
Accumulation Of Fluid In The Peritoneal Cavity: Possible Causes And Symptoms Of Ascites
What’s Causing Your Abdominal Pain And How To Treat It
Pelvic Varicocele: What It Is And How To Recognise The Symptoms
Can Endometriosis Cause Infertility?
Transvaginal Ultrasound: How It Works And Why It Is Important
Candida Albicans And Other Forms Of Vaginitis: Symptoms, Causes And Treatment
What Is Vulvovaginitis? Symptoms, Diagnosis And Treatment
Vulvodynia: Causes, Symptoms And Treatment


