Juvenile gastrointestinal polyposis: causes, symptoms, diagnosis, therapy
Juvenile gastrointestinal polyposis is a rare disease characterised by juvenile hamartomatous polyps in the gastrointestinal tract
The most severe form of juvenile gastrointestinal polyposis is juvenile polyposis
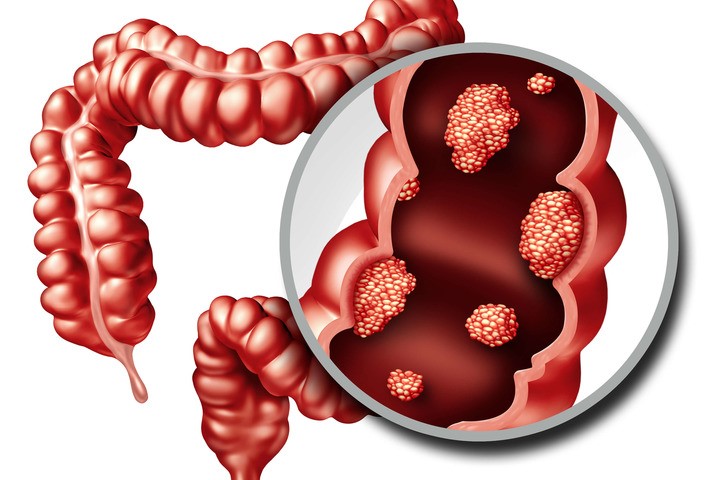
What are intestinal polyps?
Intestinal polyps are abnormal masses of tissue that form from the mucosa of the intestine (especially in the colon and rectum) and protrude into the lumen.
Although they are benign formations, over time they can become malignant (carcinoma), which is why the identification and eventual removal of intestinal polyps is an effective means of preventing colorectal cancer.
If the polyp adheres directly to the wall of the intestine, it is called a ‘sessile polyp’; if, on the other hand, it adheres by means of a pedicle, it is called a ‘pedunculated polyp’.
Depending on their specific characteristics, polyps can be of various types:
- hyperplastic and inflammatory polyps: these are of benign origin, have a low risk of transformation into malignant tumours and are often associated with ulcerative colitis, Crohn’s disease, infectious colitis and diverticulosis;
- hamartomatous polyps: these are non-neoplastic lesions frequently of familial origin;
- neoplastic or adenomatous polyps: they have a higher risk of transforming into cancer and are divided into
- tubular polyps (at lower risk of neoplastic transformation)
- villous polyps (higher risk of neoplastic transformation);
- mixed tubular-villous polyps.
Synonyms of juvenile gastrointestinal polyposis are:
- juvenile intestinal polyposis;
- juvenile polyposis syndrome.
The annual incidence is estimated to be between 1/100,000 and 1/15,000.
Age of onset
Polyps can develop at any age, from childhood to adulthood; most affected persons present with polyps from adolescence/early adulthood.
Causes and risk factors of juvenile gastrointestinal polyposis
In some cases juvenile gastrointestinal polyposis has genetic causes: mutations in the SMAD4 (18q21.1) and BMPR1A (10q22.3) genes have been identified.
To date, no genetic abnormality has been identified in approximately 60% of the cases.
Some genotype-phenotype correlations have been established: the frequency of gastric polyposis is higher in carriers of mutations in SMAD4, compared to those mutated in BMPR1A, whereas the association of juvenile gastrointestinal polyposis with hereditary haemorrhagic telangiectasia (juvenile polyposis/hereditary haemorrhagic telangiectasia syndrome) has been observed in less than a quarter of the carriers of mutations in SMAD4.
Transmission
Juvenile gastrointestinal polyposis is transmitted in an autosomal dominant manner: a disease is said to have autosomal dominant transmission when a single copy of the defective allele is sufficient for the disease to be expressed, regardless of sex (only one affected parent is needed).
The child of an affected individual has a 50% chance of being affected, i.e. 1 in 2 children is ill and can in turn transmit the disease to half of his or her children.
In this case, there cannot be a ‘healthy carrier’ (which can occur in autosomal recessive transmission): those who possess the altered allele have the disease, while those who do not possess it are healthy.
Consequently, from two healthy parents, 100% healthy children are born, whereas if both parents are sick, then 100% sick children are born.
Several types of juvenile gastrointestinal polyposis have been described, which include various differentiations based on the location of the polyps
- generalised juvenile polyposis of the upper and lower gastrointestinal tract;
- juvenile polyposis of the colon;
- juvenile polyposis of the stomach;
- juvenile polyposis of childhood (more severe).
Symptoms and signs
Regardless of subtypes, clinical signs of juvenile gastrointestinal polyposis include isolated rectal bleeding, anaemia, abdominal pain, intussusception, diarrhoea.
In juvenile colonic polyposis and generalised juvenile polyposis, rectal prolapse and spontaneous elimination of polyps from the anus may be present. Other symptoms may be growth retardation and oedema.
Diagnosis is based on:
- anamnesis;
- objective examination;
- endoscopic examination (oesophagogastroscopy and colonoscopy) with biopsy;
- histological analysis of polyps;
- molecular analysis.
The diagnosis of juvenile gastrointestinal polyposis is made on the basis of one or more of the following signs
- more than 5 juvenile polyps in the colon and/or rectum
- juvenile polyps in the digestive tract, including the stomach;
- juvenile polyps and family history of juvenile gastrointestinal polyposis.
Genetic testing
Molecular analysis may be useful to confirm the diagnosis of juvenile gastrointestinal polyposis in carriers of mutations in the SMAD4 and BMPR1A genes.
Differential diagnosis
The differential diagnosis arises with diseases characterised by similar clinical pictures, including:
- Cowden syndrome;
- Bannayan-Riley-Ruvalcaba;
- familial adenomatous polyposis;
- Peutz-Jeghers syndrome.
Treatment includes:
- routine colonoscopy: periodic colonoscopies are performed to detect the formation of new polyps;
- polypectomy: a medical procedure in which intestinal polyps are extracted endoscopically;
- partial colectomy: in the case of numerous and bulky polyps in a given area of the intestine, the entire affected part of the intestine is surgically removed
- total colectomy: consists of the removal of the entire colon, either laparoscopically or by open surgery. Laparoscopy is generally preferable to standard surgical techniques and allows a faster and less painful recovery of the patient.
The prognosis of juvenile gastrointestinal polyposis is based on the risk of developing cancer of the gastrointestinal tract or pancreas after the age of 20 years
The cumulative risk of developing cancer in patients with juvenile gastrointestinal polyposis is 20% at age 35 and 68% after age 60.
The risk of cancer is higher among persons with generalised juvenile polyposis.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Ulcerative Colitis: What Are The Typical Symptoms Of The Intestinal Disease?
Wales’ Bowel Surgery Death Rate ‘Higher Than Expected’
Irritable Bowel Syndrome (IBS): A Benign Condition To Keep Under Control
Intestinal Infections: How Is Dientamoeba Fragilis Infection Contracted?
Study Finds Link Between Colon Cancer And Antibiotic Use
Colonoscopy: More Effective And Sustainable With Artificial Intelligence
Colorectal Resection: In Which Cases The Removal Of A Colon Tract Is Necessary
Intestinal Polyps: Diagnosis And Types
Colonoscopy: What It Is, When To Do It, Preparation And Risks
Transvaginal Ultrasound: How It Works And Why It Is Important
Rare Diseases: Nasal Polyposis, A Pathology To Know And Recognise


