Keratoconus: what is it?
Keratoconus – from the Greek keratos: “cornea” and konos: “cone”, often abbreviated in the medical field as KC – is a degenerative disease which involves a progressive deformation of the cornea, which undergoes a progressive wear and tear of the tissue which becomes thinner and everted at the apex
Keratoconus: the causes
A multifactorial pathogenesis is recognized as both genetic and environmental factors are involved.
Due to an anomaly found in the collagen fibers that make up the corneal stroma, the cornea tends to deform progressively, stretching outwards, thinning, thus assuming that characteristic shape that gives the disease its name: the cone.
The cornea therefore loses its normal spherical shape.
In the most serious cases of keratoconus, the cornea even ends up losing its natural transparency, presenting widespread opacity due to the presence of micro-scars due to an altered arrangement of corneal proteins.
Keratoconus: symptoms
Keratoconus can affect only one or both eyes, although the symptoms can also be perceived by only one of the two interested parties, in this case the disease will be defined as “in an asymmetric bilateral form”.
Keratoconus begins to develop in adolescence, with small, almost imperceptible changes in the cornea.
With age, the disease tends to degenerate, causing the following symptoms:
- distorted vision
- photophobia (particular sensitivity to light)
- mild eye irritation
- blurring of vision
- monocular polyopia (double vision with one eye closed)
- reduced night vision
- worsening of myopia and astigmatism due to keratoconus
- frequent changes in eyeglass prescription
- inability to wear contact lenses
Typically, keratoconus degeneration occurs between the ages of 10 and 20, it can slowly progress up to 35-40 years before stabilizing.
In rare and particular cases, however, keratoconus can degenerate rather rapidly, causing the appearance of edema and corneal scars, which will further blur the vision.
In this case, it is “acute keratoconus”.
Keratoconus: the diagnosis
The first symptom that may lead to suspect the presence of keratoconus is the reduction of vision due to progressive and irregular predominantly myopic astigmatism.
When this symptomatology occurs, it will be advisable to consult a specialized ophthalmologist, as he is the only one able to correctly diagnose the possible presence of keratoconus.
Timely diagnosis is in fact essential to counteract keratoconus, so that it has no way of degenerating until it reaches serious and worrying stages.
The first tests that are carried out to diagnose the possible presence of keratoconus are:
Retinoscopy
This exam is necessary to evaluate the projection and refraction of a beam of light on the patient’s retina, so as to be able to evaluate how it focuses on the back of the eye.
The result of the typical “scissors” beam will highlight the presence of keratoconus.
Slit lamp examination
If the retinoscopy reveals the suspicion of keratoconus, the slit lamp examination will be performed.
Also in this case, the ophthalmologist will direct a beam of light into the patient’s eye and – through the use of a low power microscope – will visualize the ocular structures in search of defects in the cornea or in other parts of the eye. eye.
Through this examination, the ophthalmologist can identify some typical signs affecting the various corneal components in particular in the corneal stroma (for example the vertical tension lines in the stroma known as “Vogt’s streaks”) or other additional signs such as increased visibility of the nerves corneal lesions and “Fleisher’s iron ring”, a consequence of hemosiderin deposition deep in the epithelium and Bowman’s layer at the base of the cone.
This test is generally performed by administering the patient a mydriatic eye drop, which dilates the pupil so as to allow a better view of the back of the cornea.
Keratometry
This examination consists in the projection of a series of concentric rings on the cornea in order to evaluate the refraction of the light beams and highlight any disturbances in the curvature of the cornea.
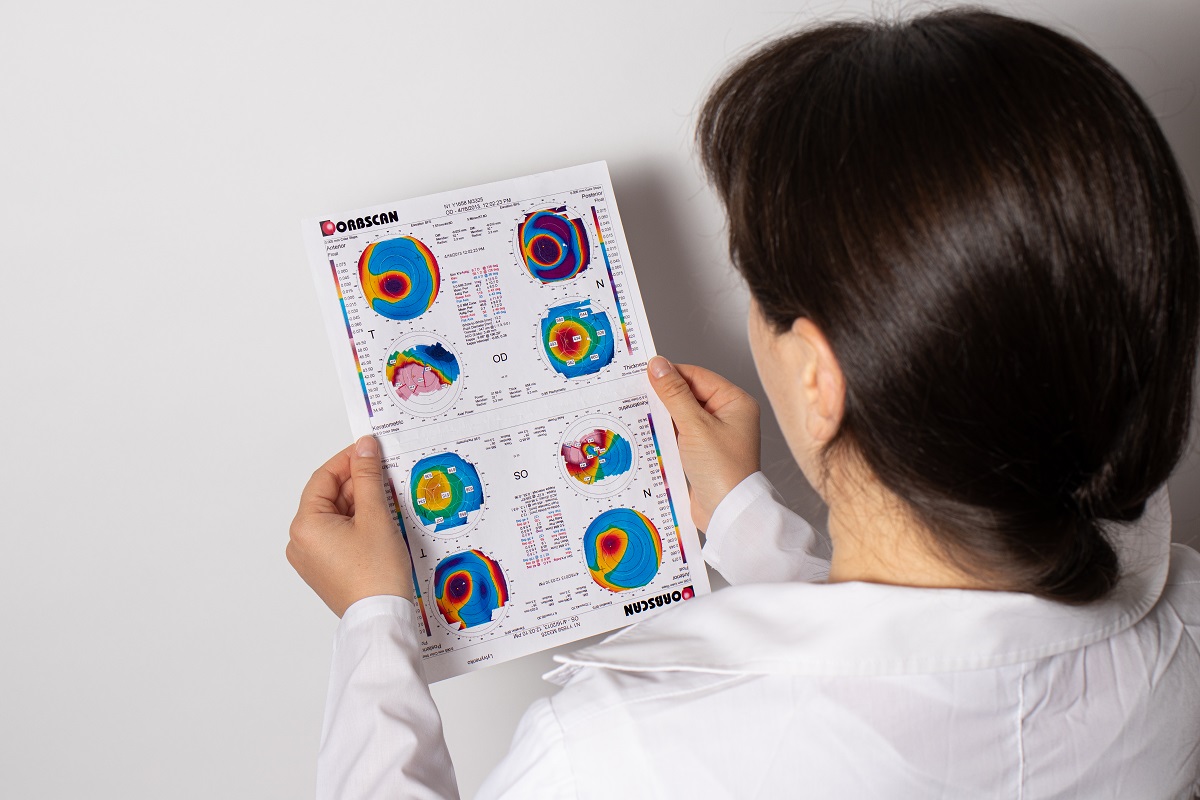
Corneal topography
Corneal topography – also known as corneal mapping – consists of a diagnostic test that analyzes and maps the topographic surface of the eye.
This examination is performed thanks to the use of a computerized optical instrument that projects light patterns on the cornea to postpone its thickness.
Corneal pachymetry
The test that measures corneal thickness, necessary to evaluate the progression of corneal ectasia.
Corneal tomography
Investigation method that analyzes the anterior surface and the posterior corneal surface highlighting the deformation of the cornea even in cases of posterior wear.
It is very useful in surgical planning and in evaluating the depth of treatment after cross-linking. It is also the most reliable test for evaluating the thickness map of the affected cornea.
Confocal microscopy
It allows ultrastructural evaluation of the cornea and is useful in the planning and choice of surgical treatment in more advanced cases
Keratoconus: therapy
The treatment of keratoconus depends on the extent of the deformation itself and on how much this is in a slow or rapid degeneration phase.
During the early stages of keratoconus – when this is still mild – the visual defect can be treated by using eyeglasses with specific lenses to correct the visual defect generated by keratoconus.
Alternatively, even the appropriate contact lenses – rigid or semi-rigid – may be sufficient to correct the visual defect.
Unfortunately, these devices will only be transient as keratoconus – as a degenerative disease – could quickly make eyeglasses and contact lenses no longer sufficient to correct the visual disturbance.
Devices such as rigid gas permeable contact lenses, piggy-black contact lenses, scleral and semi-scleral contact lenses will then be needed.
In the moment of maximum progression of keratoconus, that is when the disease begins to reach advanced stages, neither the glasses nor the contact lenses just mentioned can remedy the problem.
In these cases we will appeal to corneal inserts: small semicircular devices – inserted through a small surgical operation – which are placed in the peripheral part of the cornea to try to restore the normal hemispherical shape of the anterior surface of the eye.
As an alternative to inserting corneal inserts, the ophthalmologist could opt for corneal reticulation (Cross Linking): a procedure which consists in strengthening the corneal tissue thanks to a substance – activated by a special UV lamp – which allows to promote the strengthening of the collagen fibers of the stromal layer of the cornea.
However, when keratoconus occurs in its most acute and by now irreversible stage, the surgical choice falls on keratoplasty techniques or in the replacement of a more or less large portion of pathological corneal tissue with a healthy portion of donor cornea.
This operation is only necessary in 10/20% of cases of keratoconus, when this now has a structurally compromised cornea with penalizing visual acuity.
The procedure consists of removing the damaged cornea and replacing it with cornea from a healthy donor.
We will talk about lamellar keratoplasty where only the pathological corneal layers are replaced, leaving the healthy ones in situ, and perforating keratoplasty where the pathological cornea is replaced in its entirety.
Visual recovery after corneal transplantation will require longer times and the postoperative course will be aimed at preventing the onset of infections and eventual rejection of the transplanted cornea through the use of systemic and local cortisone and antibiotics.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Keratoconjunctivitis: Symptoms, Diagnosis And Treatment Of This Inflammation Of The Eye
Corneal Keratoconus, Corneal Cross-Linking UVA Treatment
Keratoconus: The Degenerative And Evolutionary Disease Of The Cornea
Burning Eyes: Symptoms, Causes And Remedies
What Is The Endothelial Count?
Ophthalmology: Causes, Symptoms And Treatment Of Astigmatism
Asthenopia, Causes And Remedies For Eye Fatigue
Blepharitis: What Is It And What Does Chronic Inflammation Of The Eyelid Entail?
Inflammations Of The Eye: Uveitis
Myopia: What It Is And How To Treat It
Presbyopia: What Are The Symptoms And How To Correct It
Nearsightedness: What It Myopia And How To Correct It
Blepharoptosis: Getting To Know Eyelid Drooping
Lazy Eye: How To Recognise And Treat Amblyopia?
What Is Presbyopia And When Does It Occur?
Presbyopia: An Age-Related Visual Disorder
Blepharoptosis: Getting To Know Eyelid Drooping
Rare Diseases: Von Hippel-Lindau Syndrome
Rare Diseases: Septo-Optic Dysplasia
Diseases Of The Cornea: Keratitis
Dry Eye Syndrome: How To Protect Your Eyes From PC Exposure
Dry Eyes In Winter: What Causes Dry Eye In This Season?
Why Do Women Suffer From Dry Eye More Than Men?
Autoimmune Diseases: The Sand In The Eyes Of Sjögren’s Syndrome
Dry Eye Syndrome: Symptoms, Causes And Remedies
How To Prevent Dry Eyes During Winter: Tips
Blepharitis: The Inflammation Of The Eyelids
Blepharitis: What Is It And What Are The Most Common Symptoms?
Stye, An Eye Inflammation That Affects Young And Old Alike
Blurred Vision, Distorted Images And Sensitivity To Light: It Could Be Keratoconus
Stye Or Chalazion? The Differences Between These Two Eye Diseases
Blepharoptosis: Getting To Know Eyelid Drooping
Lazy Eye: How To Recognise And Treat Amblyopia?



