Mediterranean anaemia: diagnosis with a blood test
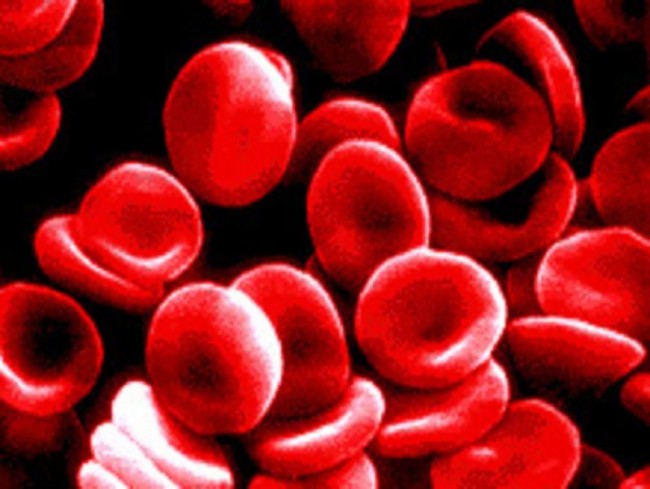
A malfunction of the red blood cells is at the root of Mediterranean anaemia: let’s better understand what it is and how to diagnose it
The disease was typically present among populations living in marshy or swampy areas, infested with malaria for centuries, such as: islands, southern regions, Po delta.
The reason for this lies in the fact that, in thalassemics, the abnormality of the red blood cells hinders the reproduction of the malaria plasmodium, making them more resistant to this disease and allowing, over the years, a sort of natural selection of people with thalassemia in certain areas of Italy.
What is Mediterranean anaemia or thalassaemia?
Mediterranean anaemia is synonymous with thalassaemia, a hereditary blood disorder due to reduced or absent synthesis of one of the chains of haemoglobin, the protein responsible for transporting oxygen throughout the body.
The name thalassaemia derives from the Greek thàlassa, ‘sea’, and αἷμα, àima, ‘blood’, and was chosen because of the widespread occurrence of this disease in the Mediterranean region.
Mediterranean anaemia, thalassaemia minor and major: how to recognise them
Depending on the form of the disease, symptoms range from extremely complex to absent.
The most common form is thalassaemia minor, which is asymptomatic and has a higher percentage of symptoms. It is not a problem in everyday life and is diagnosed by common laboratory tests.
The more severe form is known as thalassaemia major or Cooley’s disease, a condition that involves dependence on blood transfusions.
In between is thalassaemia intermedia, whose symptoms vary widely.
It can manifest itself with mild or moderate symptoms or in a more violent form, similar to Cooley’s disease.
Thalassaemia minor is characterised by a wide spread and the absence of symptoms: the diagnosis of Mediterranean anaemia is made by blood test.
The healthy carrier and transmission to offspring
Individuals suffering from this disease have red blood cells that are smaller than normal, the so-called thalassaemia.
This is why it is called microcytic anaemia.
What usually affects people with this form of the disease is that it can be passed on to their children.
The patient is in fact a healthy carrier, and his or her defective gene can be passed on to the unborn child.
This is a fundamental factor to take into account for possible pregnancies.
Marriage with a partner who is also a healthy carrier of beta thalassaemia defines
- a 25% chance of giving birth to a child with thalassaemia major.
- In 50% of cases, the unborn child will be a healthy carrier of the disease.
- while the remaining 25% will not inherit any defective genes.
Recommended tests in pregnancy for diagnosis of Mediterranean anaemia
During pregnancy, molecular tests can be used to determine whether the baby will be born with Mediterranean anaemia.
In this case the prenatal tests to be carried out are:
- amniocentesis, which is usually carried out between the 16th and 18th week of pregnancy
- chorionic villus sampling, which should be carried out between the 11th and 13th week of pregnancy.
- Blood transfusion and bone marrow transplantation: when they are needed
Thalassaemia minor is almost always detected by chance during routine examinations.
No specific therapy is needed for the minor form, unless the patient complains of weakness and paleness: then anti-anaemic drugs (folic acid, vitamin B12) can be prescribed, while iron is usually present in the blood at normal values.
In the intermediate form, anaemia sometimes requires occasional transfusions of red blood cells, while in the major form haemotransfusions of haematia (red blood cells, ed.) are almost constant: in rare cases a bone marrow transplant may even be planned.
Sometimes, especially in those who receive haemotransfusions, the amount of iron in the blood is too high and a therapy to reduce iron levels must be introduced.
On the other hand, people with thalassaemia minor should lead a completely normal life, with a balanced diet, preferably rich in folic acid (especially green leafy vegetables, pulses, oranges, etc.).
Read Also:
Symptoms Of Coeliac Disease: When To Consult A Doctor?
Increased ESR: What Does An Increase In The Patient’s Erythrocyte Sedimentation Rate Tell Us?
Anaemia, Vitamin Deficiency Among Causes


