Osteochondrosis: definition, causes, symptoms, diagnosis and treatment
Osteochondrosis or osteochondritis refers to a degenerative syndrome of the bones: young people and sportsmen or those subject to frequent trauma to the joints are particularly affected
This clinical condition involves fragmentation of bone ends, probably through tissue necrosis.
If the diagnosis is made in time, the pathology can be managed with a non-invasive therapeutic intervention, which is different in the case of a late diagnosis: we will see what to do in this case later.
What is osteochondrosis
The term osteochondrosis does not refer to a single disease, but to a series of pathologies in which there is a fragmentation – bony or cartilaginous – of the bone extremities, without distinction between long and short bones.
In practice, there is a bone lesion that separates a small fragment of subchondral bone – the portion of bone just below the cartilage – and cartilage from the main bone.
In this way, a small free osteocartilaginous body is formed that causes more or less intense pain and is called by a curious medical term, namely joint mouse.
Although all the bones of the body can be affected, those most affected are precisely the bones that are part of the joint because of the greater stresses to which they are subjected.
In particular, osteochondrosis occurs in the knee, hip, ankle and elbow joints.
Men are more affected by osteochondrosis than women, and it occurs in particular in children and young people under the age of 20, due to the intense ossification activity.
If osteochondrosis occurs due to growth causes, it tends to resolve spontaneously at the end of skeletal maturity; it is different when it occurs in adults – in particular sportspeople or those who carry out rather heavy work: it will be up to the doctor to intervene in the manner he or she considers most appropriate.
The stages of osteocartilage injury
Except for a few fortuitous events, osteocartilaginous injuries follow a rather slow course, in which 4 stages can be distinguished: in the first two, the prognosis is good and the injuries are considered stable, in the other two, however, the prognosis is not favourable and the injuries are unstable.
Let us look specifically at the characteristics of the 4 stages:
- At the point of injury there is a small flattening of the bone.
- One begins to see the fragment distinctly and there is a small distancing with the bone.
- The fragment is now practically separated, the space separating it from the bone is increasing.
- The osteocartilaginous fragment is now free in the joint, meaning that it is completely separated from the original bone.
What are the causes
There has been debate for years about the possible causes of the separation of a small osteocartilaginous portion.
Today, the scientific community agrees that the cause of osteochondrosis is necrotic degeneration.
In practice, the cells of the bone end die, causing first the weakening and then the fragmentation of the affected portion.
At the origin of necrosis there is most probably an interruption of blood flow due to several factors:
1- Ischaemia
2- Bone trauma
3- In developmental age, it could be intense ossification
Let’s not forget that genetic predisposition factors and alterations in endrocrine activity are also at the root of tissue necrosis resulting in osteochondrosis.
Symptoms
There are certain symptoms that suggest a diagnosis of osteochondrosis, although they could be confused with other pathological conditions because they are rather generic.
These are pain, swelling, effusion and joint blockage.
Obviously, in the early stages of the injury, the symptoms will be much milder than in the late stages, and it takes months – in some cases even years – for the symptoms of osteochondrosis to become intense and continuous, to the extent that they affect the quality of life.
The diagnosis of osteochondrosis
Let us imagine that we have osteochondrosis in the knee: given the generality of the symptoms, we could easily confuse it with a meniscus rupture or other clinical pathological conditions affecting the joint.
For this reason, if we suspect that we are suffering from osteochondrosis, we must speak to our general practitioner, who will direct us to the appropriate specialist.
It is important that there is an early diagnosis. Only then will it be possible to intervene in the least invasive way possible and nip the lesion in the bud.
At the time of the visit, the specialist will make an analysis of the joint motility: reduced motility may raise the suspicion of pathology.
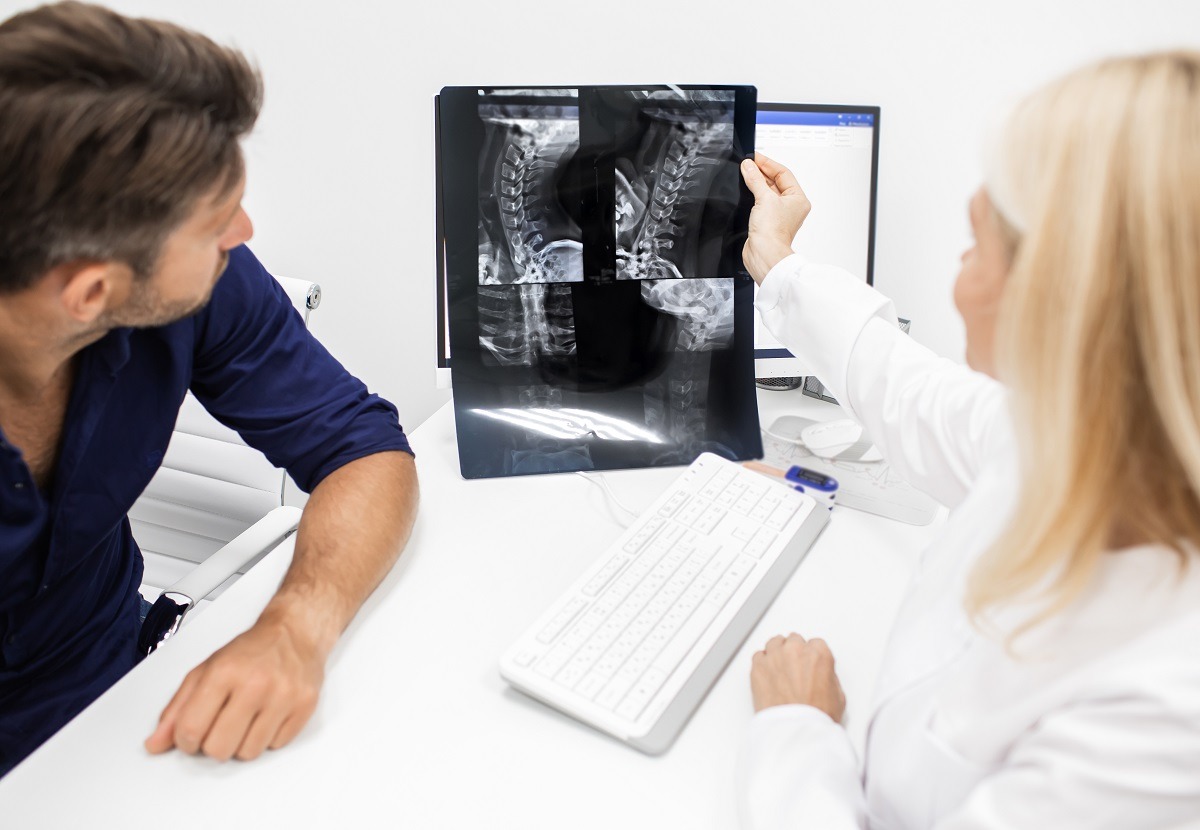
The doubt may be confirmed by an MRI scan, which ‘photographs’ the extent of the lesion in order to plan an effective therapy.
However, other diagnostic tests may also be prescribed, such as an X-ray and a CT (computed axial tomography) scan.
Let’s take a closer look at what they are used for:
– Radiography. It allows all the bones to be observed, it could therefore show a separate bone fragment or a joint mouse.
– CT scan. Like MRI, it allows us to ‘photograph’ the affected joint, identifying any fragmentation.
Once the diagnosis of osteochondrosis has been established, the recommended therapy will differ depending on the severity of the lesion
In the first two stages of the injury and in cases of osteochondrosis caused by growth, conservative therapy is preferred.
In practice, one will have to rest for 6-8 weeks, sometimes even immobilised with a cast and, in the case of lower limb pathology, use crutches for walking.
In this case, physiotherapy is also recommended.
Sometimes supportive drug therapy is necessary to relieve symptoms such as pain and swelling.
In itself, drug therapy does not intervene in the causes, so it cannot be considered decisive.
The drugs administered are analgesics and non-steroidal anti-inflammatory drugs.
In unstable or stable cases that have not benefited from conservative treatment, surgery is necessary.
The operation is performed arthroscopically and aims to recover the fragments, either partially or totally free in the joint.
The affected cartilage component will then have to be reconstructed with a transplant of chondrocytes, cells capable of producing cartilage.
Complications
Obviously, the better the prognosis, the lower the chance of complications.
The prognosis depends not only on the state of evolution of the injury, but also on the age of the patient, the underlying causes, which joint is affected, and whether conservative therapy has already been followed.
In any case, it is possible that there may be unforeseen and unwanted complications, such as chronic pain, arthritis or reduced function of the affected joint.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Osteoporosis: How To Recognise And Treat It
About Osteoporosis: What Is A Bone Mineral Density Test?
Osteoporosis, What Are The Suspicious Symptoms?
Osteoporosis: Definition, Symptoms, Diagnosis And Treatment
Back Pain: Is It Really A Medical Emergency?
Osteogenesis Imperfecta: Definition, Symptoms, Nursing And Medical Treatment
Exercise Addiction: Causes, Symptoms, Diagnosis And Treatment
Rotator Cuff Injury: What Does It Mean?
Tendon Injuries: What They Are And Why They Occur
Elbow Dislocation: Evaluation Of Different Degrees, Patient Treatment And Prevention
Cruciate Ligament: Watch Out For Ski Injuries
Sport And Muscle Injury Calf Injury Symptomatology
Meniscus, How Do You Deal With Meniscal Injuries?
Meniscus Injury: Symptoms, Treatment And Recovery Time
First Aid: Treatment For ACL (Anterior Cruciate Ligament) Tears
Anterior Cruciate Ligament Injury: Symptoms, Diagnosis And Treatment
Work-Related Musculoskeletal Disorders: We Can All Be Affected
Patellar Luxation: Causes, Symptoms, Diagnosis And Treatment
Arthrosis Of The Knee: An Overview Of Gonarthrosis
Varus Knee: What Is It And How Is It Treated?
Patellar Chondropathy: Definition, Symptoms, Causes, Diagnosis And Treatment Of Jumper’s Knee
Jumping Knee: Symptoms, Diagnosis And Treatment Of Patellar Tendinopathy
Symptoms And Causes Of Patella Chondropathy
Unicompartmental Prosthesis: The Answer To Gonarthrosis
Anterior Cruciate Ligament Injury: Symptoms, Diagnosis And Treatment
Ligaments Injuries: Symptoms, Diagnosis And Treatment
Knee Arthrosis (Gonarthrosis): The Various Types Of ‘Customised’ Prosthesis
Rotator Cuff Injuries: New Minimally Invasive Therapies
Knee Ligament Rupture: Symptoms And Causes
MOP Hip Implant: What Is It And What Are The Advantages Of Metal On Polyethylene
Hip Pain: Causes, Symptoms, Diagnosis, Complications, And Treatment
Hip Osteoarthritis: What Is Coxarthrosis
Why It Comes And How To Relieve Hip Pain
Hip Arthritis In The Young: Cartilage Degeneration Of The Coxofemoral Joint
Visualizing Pain: Injuries From Whiplash Made Visible With New Scanning Approach
Coxalgia: What Is It And What Is The Surgery To Resolve Hip Pain?
Lumbago: What It Is And How To Treat It
Lumbar Puncture: What Is A LP?
General Or Local A.? Discover The Different Types
Intubation Under A.: How Does It Work?
How Does Loco-Regional Anaesthesia Work?
Are Anaesthesiologists Fundamental For Air Ambulance Medicine?
Epidural For Pain Relief After Surgery
Lumbar Puncture: What Is A Spinal Tap?
Lumbar Puncture (Spinal Tap): What It Consists Of, What It Is Used For
What Is Lumbar Stenosis And How To Treat It
Lumbar Spinal Stenosis: Definition, Causes, Symptoms, Diagnosis And Treatment
Cruciate Ligament Injury Or Rupture: An Overview
Haglund’s Disease: Causes, Symptoms, Diagnosis And Treatment


