Pneumocystis carinii pneumonia: clinical picture and diagnosis
Pneumocystis carinii pneumonia, general features: in the first decade of the AIDS epidemic, Pneumocystis carinii pneumonia (PCP) was the most frequent of the major opportunistic infections, affecting about 80% of patients with severe HIV-related immunodeficiency
The number of PCP cases then decreased during the 1990s, initially as a result of the use of primary prophylaxis in high-risk (i.e. CD4) patients.
Pneumocystis carinii (PC) is a micro-organism approximately 1.5-5 microns in size
It was originally classified as a protozoan based on its morphological characteristics and sensitivity to antiprotozoal drugs; however, more recent genetic studies suggest that PC belongs to the fungal genus.
It is ubiquitous in nature, although there may be differences in its geographical distribution.
Infection is established when the pathogen reaches the pulmonary alveoli, where it replicates as an extracellular parasite (it does not invade cells or tissues).
The involvement of the pulmonary interstitium leads to a reduction in gas exchange, resulting in reduced oxygen availability to the body.
Clinical picture and diagnosis of Pneumocystis carinii pneumonia
The typical onset of symptoms is fever, non-productive cough and dyspnoea (difficulty breathing); tachycardia, tachypnoea and sometimes cyanosis (purplish discolouration of the skin and mucous membranes, caused by oxygen deficiency, and usually more evident at the lips and subungual bed) are also usually present.
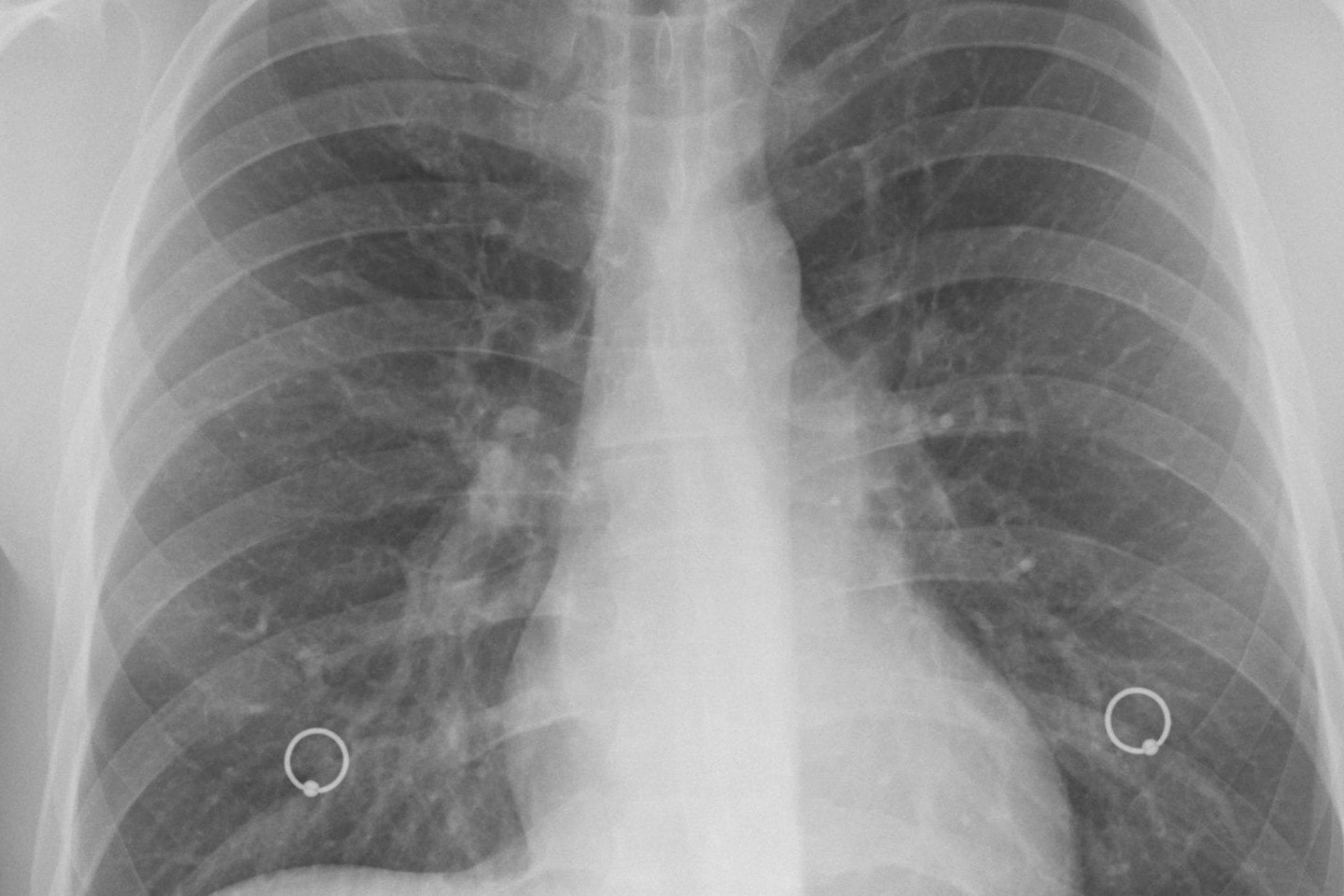
A chest X-ray shows a typical picture of interstitial or alveoli-interstitial pneumonia; haemogasanalysis usually shows a reduction in arterial blood oxygenation.
These parameters (clinical picture, radiography and reduced oxygenation of the blood) allow, in an HIV-positive patient with CD4 Presumptive diagnosis of PCP (i.e. without direct demonstration of the pathogen).
The diagnosis of certainty is made by direct detection of PCP on the induced sputum (i.e. collected after areosol with saline solution for 5-10 minutes), with a diagnostic sensitivity of 30-90%, or on bronchoalveolar lavage fluid after bronchoscopy, which is diagnostic in 98-100% of cases; the diagnosis can also be made by histological examination of transbronchial lung biopsy (diagnostic sensitivity of 90-95%).
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Kaposi’s Sarcoma: Discover What It Is
Pneumonia: Causes, Treatment And Prevention
Pneumothorax And Pneumomediastinum: Rescuing The Patient With Pulmonary Barotrauma
Bronchitis And Pneumonia: How Can They Be Distinguished?
AIDS, Difference Between HIV1 And HIV2
HIV: How Soon Do Symptoms Appear? The 4 Stages Of Infection
Endotracheal Intubation: What Is VAP, Ventilator-Associated Pneumonia


