Pneumothorax and haemothorax: trauma to the thoracic cavity and its consequences
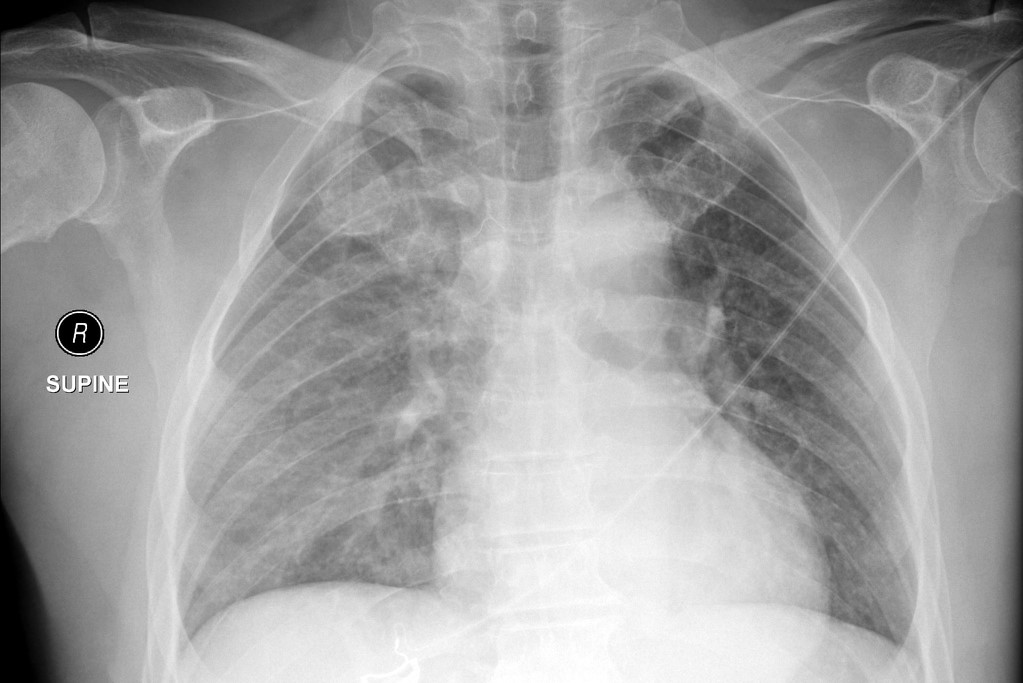
Pneumothorax and Hemothorax are collections of abnormal material (air and blood, respectively) within the chest (thoracic) cavity, in the space normally occupied by the tissue of the lungs
They are common complications of blunt or penetrating trauma to the chest.
This section will review the types, causes, and basic management of pneumothorax and hemothorax at the EMT level.
Pneumothorax
Pneumothorax has three unique presentations; simple, open, and tension.
Each involves the influx of air into the normally closed chest cavity with a resulting decrease in the ability for the affected lung to expand.
The three subtypes have unique elements of their presentations, management, and expected outcome.
SIMPLE PNEUMOTHORAX:
Occurs when a hole in the visceral pleura allows air to escape the lung and collect in the pleural space, i.e., a hole in the lining over the lung.
Holes in the pleura generally occur secondary to a fractured rib which directly lacerates the pleura or when a bleb in a patient with emphysema ruptures.
VISIT SPENCER’S STANDS AT EMERGENCY EXPO
“Paper Bag Syndrome”:
Blunt trauma that occurs when a patient is holding their breath at full inspiration may also “pop” the pleura like a balloon as the alveolar pressure rises past what the pleura can contain, i.e., alveolar rupture.
Management of a simple pneumothorax generally only requires the administration of oxygen via non-rebreather @ 12 to 15 LPM, as patients only have minor dyspnea.
To rule out other complications of trauma, IV access should be obtained, patients should be placed on cardiac monitors, pulse oximetry, and in the rare case that positive pressure ventilation is needed, end-tidal CO2 monitoring.
OPEN PNEUMOTHORAX:
Occurs when a hole in the chest wall and pleura allows air to collect in the pleural space, normally a hole greater than the size of a nickel.
These wounds are almost exclusively secondary to penetrating trauma and are often called “sucking chest wounds” after the noises they make when blood leaving the circulation mixes with air being pulled into the wound as the patient inhales.
These wounds have a high rate of conversion to tension pneumothorax and/or hemothorax.
Hemostasis may be impossible to maintain due to the inability to put pressure on the inner surface of the wound.
This often results in the symptoms of mild to severe hemorrhage in addition to the expected symptoms of poor ventilation.
Management of open pneumothorax is focused around the placement of an “occlusive dressing.”
By placing the dressing, taping down three sides and leaving one end open to the air, you create a one-way valve that seals the chest upon inspiration but allows accumulated air and blood to leave the lung on expiration.
Air can still accumulate if the lungs’ visceral pleura is also damaged, lifting the dressing off of the wound temporarily will allow any developing tension pneumothorax to decompress.
Pneumothorax can progress rapidly, requiring you to place a gloved hand over the wound until an occlusive dressing can be applied.
The remainder of management is similar to an open pneumothorax, oxygen via non-rebreather, cardiac monitors, pulse oximetry, and end-tidal CO2 monitoring are indicated.
Frequent re-assessment for the development of tension pneumothorax (hypotension, JVD, and decreased breath sounds) and blood loss (headache, cold extremities, diaphoresis, and weak pulses) is paramount.
TENSION PNEUMOTHORAX:
Is a true emergency, and results from a hole in the lung or chest wall acting as a one-way valve, allowing air to enter the thorax with inspiration and preventing it from exiting with expiration.
QUICK TIPS: Characteristic signs of a tension pneumothorax are:
- Jugular Vien Distention (JVD)
- Hyper-resonance on one side
- Tachycardia
- Hypotension
Tension pneumothorax is a progressive condition that worsens as each breath increases the pressure inside the chest, further deflating the lung.
As the pressure increases the mediastinum is pushed to the opposite side.
The mediastinal deviation and pressure work together to decrease venous return to the heart, dramatically dropping preload and leading to distention of the neck veins, weak pulses, and hypotension.
Eventually, the dramatic mediastinal shift leads to a deviation of the trachea away from the affected side.
This combination of insults to the cardio-respiratory system leads to dramatic hypoxia and obstructive shock.
Management of tension pneumothorax begins with its identification, the classical symptom of tracheal deviation should not be relied upon as it is a very late finding.
A progressive compromise of circulation combined with unequal lung sounds on exam should prompt the consideration of tension pneumothorax and its primary field treatment, needle decompression.
Depending on your jurisdiction, needle decompression may be available to providers trained at the EMT, AEMT, or Paramedic level.
Providing 100% oxygen via non-rebreather mask or bag-valve-mask is indicated regardless of needle decompressions availability.
All patients with suspected tension pneumothorax should be seen at an emergency department even if decompression relieves symptoms, as recurrence of tension is almost guaranteed without further treatment.
Needle Decompression Procedure
The needle decompression procedure is indicated whenever a tension pneumothorax is suspected based on clinical symptoms, the procedure for doing so is outlined below.
Gather Equipment-A large (14 gauge or larger) angiocath works well. It is imperative that you use at least a 3 ¼” long needle.
For the procedure to be effective you must be able to puncture into the pleural cavity.
Some patients may have a thick (2-3cm) chest wall.
There are several commercial devices on the market that are specifically designed for needle decompression.
Most include a flutter valve or one-way valve device on them.
These valves act to allow air to escape but not reenter the pleural cavity.
A finger cut from a latex glove or a condom works also.
Using a flutter valve on the needle is not as imperative as using a long enough needle.
The likelihood of enough air reentering via the needle to really affect the patient is small.
Identify Landmarks-You may use the 2nd intercostal (ICS) space at the midclavicular line or the 5th-6th ICS at the anterior axillary line to perform the procedure.
Take care to note the proper site and landmarks.
The 5th ICS is roughly the nipple line. Pick your site and clean the area with alcohol or betadine.
Insert the needle on the superior aspect of the rib.
Remember that a nerve, vein, and artery run on the inferior aspect.
You may puncture the skin holding the needle perpendicularly; If you hit a rib “tunnel” slightly to puncture over the superior aspect.
As the needle enters the pleural space you should hear a hiss or rush of air as the air under tension is released.
Secure the needle or device to the chest wall and if available attach a flutter valve.
Anticipate placement of a chest tube as soon as qualified personnel and equipment are available.
Continue to monitor the patient for dyspnea or return/worsening of symptoms.
If the patient deteriorates further consider repeating the procedure at another site.
The previously placed needle or device could have clotted off.
Hemothorax
Hemothorax is the filling of the lungs of the chest cavity with blood, this condition has both strong similarities and differences from pneumothorax.
SIMILARITIES TO PNEUMOTHORAX:
Hemothorax can result from any injury to the chest, as with pneumothorax, it often results from internal fractures of the ribs.
Puncture wounds that result in an open pneumothorax can also develop into a hemothorax if more blood accumulates than air.
The symptoms of hemothorax result from the displacement of lung tissue by blood, compromising ventilatory capacity.
If allowed to progress a tension hemothorax can present, these are largely identical in presentation as tension pneumothorax.
As with pneumothorax, hypoxia, difficulty breathing, and decreased or absent lung sounds on the affected side are the key symptoms.
DIFFERENCES FROM PNEUMOTHORAX:
The majority of patients that present with a traumatic pneumothorax will have some blood in the chest cavity, the differentiator that makes it a hemothorax is the presence of more blood than air in the chest cavity.
A sufficient amount of blood within the lung (such as from pulmonary hemorrhage) is also considered a hemothorax.
Any collection of blood that significantly displaces ventilatory capacity is termed a hemothorax.
The signs and symptoms of hemothorax are based on the reality that a dense fluid is filling the space normally occupied by the lungs as opposed to air.
This results in a chest that is dull to percussion (hypo-resonant), as opposed to tympanic (hyper-resonant).
The loss of blood into the chest cavity also results in rapid development of signs and symptoms of significant blood loss: Tachycardia, tachypnea, cold skin, diaphoresis, and eventually hypotension.
HEMOTHORAX: dull (hypo-resonance) to percussion
There is no JVD (neck veins are flat).
PNEUMOTHORAX: tympanic (hyper-resonance) to percussion
Unless there is hypovolemia, there is JVD (distended neck veins).
Although both can shift the mediastinum (trachea), the pneumothorax will do it first, because it would take A LOT of blood to build up enough to create tension (which, admittedly, would be a very late–and very bad finding: shock would come first!).
In other words, if you’re tested re: pneumo- vs hemothorax and the presence or absence of JVD is mentioned, go with
- presence = pneumothorax, and
- absence = hemothorax.
MANAGEMENT OF HEMOTHORAX: Two large-bore IVs
The Management of hemothorax is similar to pneumothorax in that maintaining the patient’s oxygenation is generally the chief concern.
Along with oxygenation, watch for signs of circulatory compromise, as the chest cavity has sufficient volume to “hide” enough blood to lead to hemorrhagic shock in nearly any patient.
Remember the principle of permissive hypotension, as excessive fluid resuscitation can wash out clotting factors and lead to further bleeding.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Airway Management After A Road Accident: An Overview
Tracheal Intubation: When, How And Why To Create An Artificial Airway For The Patient
What Is Transient Tachypnoea Of The Newborn, Or Neonatal Wet Lung Syndrome?
Traumatic Pneumothorax: Symptoms, Diagnosis And Treatment
Diagnosis Of Tension Pneumothorax In The Field: Suction Or Blowing?
Pneumothorax And Pneumomediastinum: Rescuing The Patient With Pulmonary Barotrauma
Cervical Collar In Trauma Patients In Emergency Medicine: When To Use It, Why It Is Important
KED Extrication Device For Trauma Extraction: What It Is And How To Use It
ABC, ABCD And ABCDE Rule In Emergency Medicine: What The Rescuer Must Do
Multiple Rib Fracture, Flail Chest (Rib Volet) And Pneumothorax: An Overview
Primary, Secondary And Hypertensive Spontaneous Pneumothorax: Causes, Symptoms, Treatment


