Primary, secondary and hypertensive spontaneous pneumothorax: causes, symptoms, treatment
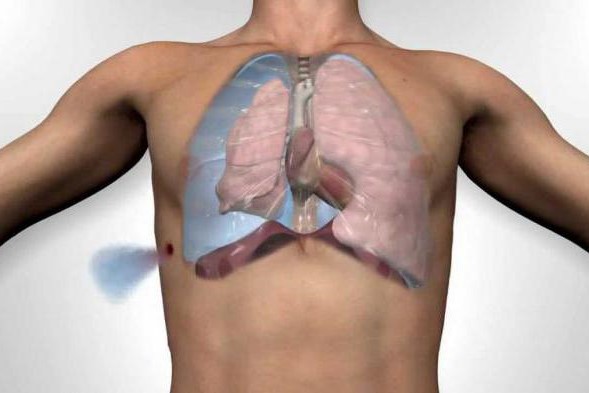
Pneumothorax (PNX) is a sudden-onset condition characterised by the presence of air in the pleural space (i.e. the virtual space between the two pleural leaflets that line the lung and chest wall)
It is caused by the rupture of a pulmonary bubble whereby air accumulates in the pleural cavity, taking away space from the lung with the consequent risk of lung collapse.
It can be spontaneous, post-traumatic or secondary to disease.
Causes of pneumothorax
Pneumothorax can be primary or secondary.
Primary spontaneous pneumothorax
The spontaneous or simple type is of unknown aetiology and often occurs in the absence of pulmonary disease.
It is frequently found in males: under 40 years of age, tall, thin, often smokers.
It is caused by the spontaneous rupture of small subpleural bullae, localised at the pulmonary apices.
It often involves the right lung and has a high probability of recurrence (50%).
Secondary spontaneous pneumothorax
Spontaneous secondary pneumothorax occurs in the context of a variety of lung diseases.
The most common is chronic obstructive pulmonary disease, which accounts for about 70% of cases.
In children, other causes are measles, echinococcosis, inhalation of a foreign body and certain congenital malformations (cystic adenomatoid malformation and congenital lobar emphysema).
11.5% of individuals with a spontaneous pneumothorax had a family member who in turn had previously had this condition.
Hereditary conditions such as Marfan syndrome, homocystinuria, Ehlers-Danlos syndrome, alpha 1-antitrypsin (leading to emphysema) and Birt-Hogg-Dubé syndrome have been linked with familial pneumothorax.
In general, these conditions cause other signs and symptoms, and pneumothorax is usually not the first event to occur.
Birt-Hogg-Dubé syndrome is caused by mutations in the FLCN gene (located on chromosome 17 p11.2), which codes for a protein called folliculin.
Mutations in the FLCN gene and lung lesions have also been identified in familial cases of pneumothorax in which other features of Birt-Hogg-Dubé syndrome are absent.
In addition to the genetic correlations just described, the HLA haplotype A2B40 is also a genetic predisposition for spontaneous pneumothorax.
Traumatic pneumothorax
A traumatic pneumothorax may result from blunt trauma or a penetrating wound in the chest wall.
The most common event is a rib fracture in which the bone stump penetrates the pleura damaging the lung tissue.
This type can also be found in explosion victims.
Certain medical procedures involving the chest, such as insertion of a central venous catheter or biopsy of lung tissue, can lead to a pneumothorax.
The administration of positive pressure ventilation, whether mechanical or non-invasive, can cause a barotrauma leading to a pneumothorax
Symptoms
Pneumothorax is manifested by sudden stabbing chest pain, which may be associated with difficulty breathing and a dry cough.
In some cases the condition may be asymptomatic.
Hypertensive pneumothorax
Hypertensive pneumothorax refers to a condition that leads to significant impairment of breathing or blood circulation.
The most common findings in people with a hypertensive pneumothorax are chest pain and difficulty breathing, often with an increased heart rate (tachycardia) and rapid breathing (tachypnoea).
This is a medical emergency that may require immediate treatment without further investigation.
Pneumothorax hypertension may occur during mechanical ventilation, in which case it may be difficult to detect, as the affected person is sedated.
Deviation of the trachea to one side and the presence of increased jugular venous pressure (dilated neck veins) are not reliable as clinical signs.
Diagnosis
The diagnosis of pneumothorax may be based on:
- chest X-ray: in order to observe the presence of air in the pleural cavity and lung collapse;
- chest CT scan: essential for detecting pathologies that may cause secondary pneumothorax and the presence of bubbles;
- specialist pneumology examination.
Chest X-ray
Chest X-ray showing a spontaneous pneumothorax.
Traditionally a chest X-ray, in a postero-anterior projection, is the most appropriate diagnostic investigation.
If the X-ray does not show a pneumothorax but there is a strong suspicion, an additional chest X-ray in a lateral projection may be necessary.
It is not unusual for the mediastinum (the structure located between the lungs and containing the heart, large blood vessels and airways) to be displaced towards the healthy lung due to pressure differences.
In a hypertensive pneumothorax, the diagnosis is mainly determined by observation of symptoms such as hypoxia and shock.
The size of the pneumothorax (i.e. the volume of air in the pleural space) can be determined with a reasonable degree of accuracy by measuring the distance between the chest wall and the lung wall.
This is relevant for treatment, as pneumothoraces of different sizes need to be managed differently.
The use of computed tomography allows a more accurate measurement of size, but its routine use in this context is not recommended.
Not all pneumothoraces are uniform.
Small amounts of fluid may be seen on the chest X-ray (hydropneumothorax), this fluid may be blood (haemopneumothorax).
In some cases, the only significant abnormality visible on radiography is the ‘deep groove sign’, in which the space between the chest wall and the diaphragm is seen enlarged due to the abnormal presence of fluid.
In addition, ultrasound is commonly used in the evaluation of people who have suffered physical trauma, for example with the FAST echo protocol.
The use of ultrasound may be more sensitive than chest X-ray in identifying a pneumothorax after closed trauma.
This technique may also provide rapid diagnosis in other emergency situations and allow quantification of the size of the pneumothorax.
Treatments
If the pneumothorax is primary, minor and the patient is not very symptomatic, it may be sufficient to keep the patient under observation in a hospital setting with clinical monitoring and chest X-ray to document its resolution.
If the lung collapse is more severe, it may be necessary to place a chest drain to allow air to escape from the pleural space and thus allow the lung to expand again.
In the case of a primary pneumothorax, surgical treatment (resection of the bullae or sclerodystrophic areas responsible for the air leakage) is arranged:
- if the pathology occurs for the first time and the lung has not re-expanded on its own;
- if, despite several days having elapsed since the placement of the drain, prolonged air leakage persists;
- in the event of recurrence.
In the case of secondary pneumothorax, on the other hand, the choice of treatment must take into account the pathology that caused it, the patient’s condition and respiratory function.
How to prevent pneumothorax?
There are no possible preventive strategies for pneumothorax, but since it has been observed that cigarette smoking, probably through an inflammatory mechanism, can promote the onset of primary pneumothorax, its cessation is recommended.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Airway Management After A Road Accident: An Overview
Tracheal Intubation: When, How And Why To Create An Artificial Airway For The Patient
What Is Transient Tachypnoea Of The Newborn, Or Neonatal Wet Lung Syndrome?
Traumatic Pneumothorax: Symptoms, Diagnosis And Treatment
Diagnosis Of Tension Pneumothorax In The Field: Suction Or Blowing?
Pneumothorax And Pneumomediastinum: Rescuing The Patient With Pulmonary Barotrauma
Cervical Collar In Trauma Patients In Emergency Medicine: When To Use It, Why It Is Important
KED Extrication Device For Trauma Extraction: What It Is And How To Use It
ABC, ABCD And ABCDE Rule In Emergency Medicine: What The Rescuer Must Do
Multiple Rib Fracture, Flail Chest (Rib Volet) And Pneumothorax: An Overview


