Pulmonary tuberculosis: medical and nursing management of the tuberculosis patient
Tuberculosis is an infectious disease that primarily affects the lung parenchyma
What is Pulmonary Tuberculosis?
Pulmonary tuberculosis (PTB) is a chronic respiratory disease common among crowded and poorly ventilated areas.
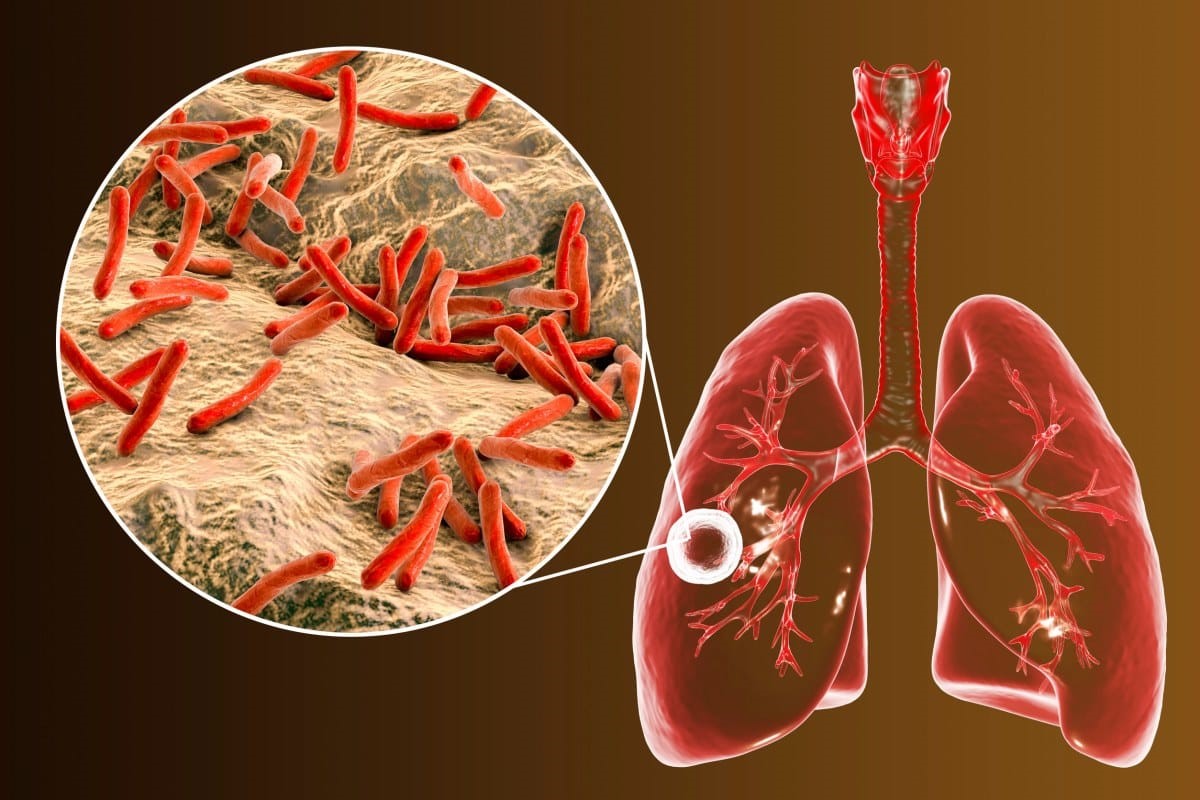
An acute or chronic infection caused by Mycobacterium tuberculosis, tuberculosis is characterized by pulmonary infiltrates, formation of granulomas with caseation, fibrosis, and cavitation.
Tuberculosis is an infectious disease that primarily affects the lung parenchyma.
It also may be transmitted to other parts of the body, including the meninges, kidneys, bones, and lymph nodes.
The primary infectious agent, M. tuberculosis, is an acid-fast aerobic rod that grows slowly and is sensitive to heat and ultraviolet light.
Pathophysiology
Tuberculosis is a highly infectious, airborne disease.
- Inhalation. Tuberculosis begins when a susceptible person inhales mycobacteria and becomes infected.
- Transmission. The bacteria are transmitted through the airways to the alveoli, and are also transported via lymph system and bloodstream to other parts of the body.
- Defense. The body’s immune system responds by initiating an inflammatory reaction and phagocytes engulf many of the bacteria, and TB-specific lymphocytes lyse the bacilli and normal tissue.
- Protection. Granulomas new tissue masses of live and dead bacilli, ate surrounded by macrophages, which form a protective wall.
- Ghon’s tubercle. They are then transformed to a fibrous tissue mass, the central portion of which is called a Ghon tubercle.
- Scarring. The bacteria and macrophages turns into a cheesy mass that may become calcified and form a collagenous scar.
- Dormancy. At this point, the bacteria become dormant, and there is no further progression of active disease.
- Activation. After initial exposure and infection, active disease may develop because of a compromised or inadequate immune system response.
Pathophysiology and Schematic Diagram for Pulmonary Tuberculosis
Classification
Data from the history, physical examination, TB test, chest xray, and microbiologic studies are used to classify TB into one of five classes.
Class 0. There is no exposure or no infection.
Class 1. There is an exposure but no evidence of infection.
Class 2. There is latent infection but no disease.
Class 3. There is a disease and is clinically active.
Class 4. There is a disease but not clinically active.
Class 5. There is a suspected disease but the diagnosis is pending.
Statistics and Incidences
Tuberculosis is a worldwide public health problem that is closely associated with poverty, malnutrition, overcrowding, substandard housing, and inadequate health care.
M. tuberculosis infects an estimated one-third of the world’s population and remains the leading cause of death from infectious disease in the world.
According to the WHO, an estimated 1.6 million deaths resulted from TB in 2005.
In the United States, almost 15,000 cases of TB are reported annually to the CDC.
After exposure to M. tuberculosis, roughly 5% of infected people develop active TB within a year.
Causes of acquiring tuberculosis include the following:
Close contact. Having close contact with someone who has an active TB.
Low immunity. Immunocompromised status like those with HIV, cancer, or transplanted organs increases the risk of acquiring tuberculosis.
Substance abuse. People who are IV/injection drug users and alcoholics have a greater chance of acquiring tuberculosis.
Inadequate health care. Any person without adequate health care like the homeless, impoverished, and the minorities often develop active TB.
Immigration. Immigration from countries with a high prevalence of TB could affect the patient.
Overcrowding. Living in an overcrowded, substandard housing increases the spreading of the infection.
Clinical Manifestations
After an incubation period of 4 to 8 weeks, TB is usually asymptomatic in primary infection.
- Nonspecific symptoms. Nonspecific symptoms may be produced such as fatigue, weakness, anorexia, weight loss, night sweats, and low-grade fever, with fever and night sweats as the typical hallmarks of tuberculosis.
- Cough. The patient may experience cough with mucopurulent sputum.
- Hemoptysis. Occasional hemoptysis or blood on the saliva is common in TB patients.
- Chest pains. The patient may also complain of chest pain as a part of discomfort.
Prevention
To prevent transmission of tuberculosis, the following should be implemented.
- Identification and treatment. Early identification and treatment of persons with active TB.
- Prevention. Prevention of spread of infectious droplet nuclei by source control methods and by reduction of microbial contamination of indoor air.
- Surveillance. Maintain surveillance for TB infection among health care workers by routine, periodic tuberculin skin testin
- Ethambutol (Myambutol). Ethambutol is a bacteriostatic agent that should be used with caution with renal disease, and has common side effects of optic neuritis and skin rash.
Nursing Management
Nursing management includes the following:
Nursing Assessment
The nurse may assess the following:
- Complete history. Past and present medical history is assessed as well as both of the parents’ histories.
- Physical examination. A TB patient loses weight dramatically and may show the loss in physical appearance.
Nursing Diagnosis
Based on the assessment data, the major nursing diagnoses for the patient include:
- Risk for infection related to inadequate primary defenses and lowered resistance.
- Ineffective airway clearance related to thick, viscous, or bloody secretions.
- Risk for impaired gas exchange related to decrease in effective lung surface.
- Activity intolerance related to imbalance between oxygen supply and demand.
- Imbalanced nutrition: less than body requirements related to inability to ingest adequate nutrients.
Nursing Care Planning & Goals
The major goals for the patient include:
- Promote airway clearance.
- Adhere to treatment regimen.
- Promote activity and adequate nutrition.
- Prevent spread of tuberculosis infection.
Nursing Interventions
Nursing interventions for the patient include:
- Promoting airway clearance. The nurse instructs the patient about correct positioning to facilitate drainage and to increase fluid intake to promote systemic hydration.
- Adherence to the treatment regimen. The nurse should teach the patient that TB is a communicable disease and taking medications is the most effective means of preventing transmission.
- Promoting activity and adequate nutrition. The nurse plans a progressive activity schedule that focuses on increasing activity tolerance and muscle strength and a nutritional plan that allows for small, frequent meals.
- Preventing spreading of tuberculosis infection. The nurse carefully instructs the patient about important hygienic measures including mouth care, covering the mouth and nose when coughing and sneezing, proper disposal of tissues, and handwashing.
- Acid-fast bacillus isolation. Initiate AFB isolation immediately, including the use of a private room with negative pressure in relation to surrounding areas and a minimum of six air changes per hour.
- Disposal. Place a covered trash can nearby or tape a lined bag to the side of the bed to dispose of used tissues.
- Monitor adverse effects. Be alert for adverse effects of medications.
Evaluation
Expected patient outcomes include:
- Promoted airway clearance.
- Adhered to treatment regimen.
- Promoted activity and adequate nutrition.
- Prevented spread of tuberculosis infection.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Tuberculin: Skin Test In Screening For Tuberculosis (TB)
Tuberculosis, Symptoms And Transmission
Who Gets Tuberculosis? Harvard Medical School Study On Immune Cell Deficiency
Médecins Sans Frontières MSF, New Strategies At Work In Eleventh Ebola Outbreak In DRC
MSF: Lifesaving TB (Tubercolosis) Medicines Still Out Of Reach For Children In High-Burden Countries
Ventilator Management: Ventilating The Patient
Three Everyday Practices To Keep Your Ventilator Patients Safe
Ambulance: What Is An Emergency Aspirator And When Should It Be Used?
The Purpose Of Suctioning Patients During Sedation
Supplemental Oxygen: Cylinders And Ventilation Supports In The USA
Basic Airway Assessment: An Overview
Respiratory Distress: What Are The Signs Of Respiratory Distress In Newborns?
EDU: Directional Tip Suction Catheter
Suction Unit For Emergency Care, The Solution In A Nutshell: Spencer JET
Airway Management After A Road Accident: An Overview
Assessment Of Ventilation, Respiration, And Oxygenation (Breathing)
Oxygen-Ozone Therapy: For Which Pathologies Is It Indicated?
Difference Between Mechanical Ventilation And Oxygen Therapy
Hyperbaric Oxygen In The Wound Healing Process


