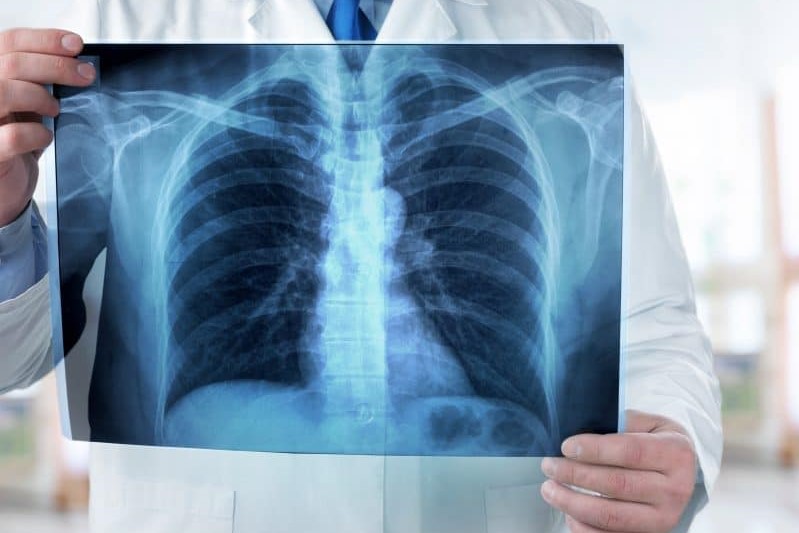
Pulmonary vasculitis: what it is, causes and symptoms
Let’s talk about pulmonary vasculitis: pulmonary vasculitis is inflammation of the blood vessels located in the respiratory tract, particularly in the lungs, which leads to chronic degeneration of the vessel walls, thickening and weakening
The causes are still unknown, although an involvement of the immune system seems certain. Vasculitides are a very broad group of diseases, among those affecting the respiratory tract are Wegener’s Granulomatosis and Churg-Strauss Syndrome.
What is pulmonary vasculitis?
There are many types of vasculitis.
Some forms have a more intense but short-lived manifestation, the acute forms, others are long-lasting and therefore chronic.
Tissue degeneration caused by inflammation results in narrowing of the blood vessels, loss of elasticity, formation of clots or weakening, which can lead to ruptures (aneurysms).
Reduced blood flow has serious consequences on organs and tissues as even the smallest vessels can no longer adequately supply the affected areas of the body with blood, oxygen and nutrients.
Among the most frequent forms of pulmonary vasculitis are:
- Wegener’s Granulomatosis is an inflammation that affects the walls of arteries and small vessels causing necrosis and granulomas, lesions related to chronic inflammation. The upper and lower respiratory tracts and the kidneys are the districts most affected by the disease, which, however, can also affect other organs
- Churg-Strauss syndrome is characterised by particularly high levels of certain white blood cells, the eosinophilic granulocytes. It is also known as allergic granulomatosis or allergic angiosis. It is often associated with asthma. After infiltrating various organs and tissues, the eosinophils cause damage by releasing toxic substances from the granules.
- Vasculitides also include microscopic polyangiitis (MPA), a systemic necrotising inflammatory vasculitis, mostly affecting small vessels (arterioles, capillaries, venules)
What are the causes of pulmonary vasculitis?
The causes of pulmonary vasculitis are still not entirely clear.
It could be an acute reaction to an infection of the respiratory tract caused by bacteria, fungi or parasites that triggers an autoimmune reaction.
The cells of the immune system incorrectly recognise the cells of the endothelium lining the walls of blood vessels as external to the body and attack them.
This chronic condition results in the formation of scar tissue (fibrous tissue), which leads to impaired blood vessel function.
What are the symptoms of pulmonary vasculitis?
People suffering from acute pulmonary vasculitis develop symptoms very quickly, within a few hours or within a few days.
When the inflammation spreads to the lungs, it can result in:
- high fever
- weakness
- muscle pain
- chest tightness
- weight loss
- muscle and joint pain
- loss of appetite
Chronic vasculitis has similar symptoms that include
- wheezing
- coughing
- difficulty breathing (dyspnoea)
- pleural effusion
- chest pain
- drumstick fingers and watch-glass nails (Digital Hippocratism)
- tiredness
- weight loss
Usually, the first signs are those of a chronic sinusitis that does not heal despite treatment, followed by otitis, a wheezing cough and ulcers in the mouth and nasal mucosa.
Vasculitis leads to significant tissue damage, haemorrhaging and a reaction that also involves the heart and results in cyanosis, respiratory failure, heart failure, oedema, blood in the sputum (haemoptysis), Raynaud’s phenomenon, syncope.
How can pulmonary vasculitis be prevented?
There are no measures to effectively prevent pulmonary vasculitis.
It is advisable to eat a balanced diet, rich in fruit, vegetables and wholegrains and low in fat, to avoid smoking and alcohol, and to exercise regularly and moderately.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
What Are Vascular Malformations
Kawasaki Syndrome, The Most Common Childhood Vasculitis
Vasculitis: Symptoms And Causes Of Horton’s Arteritis
Venous Thrombosis: From Symptoms To New Drugs
Deep Vein Thrombosis Of The Upper Limbs: How To Deal With A Patient With Paget-Schroetter Syndrome
Venous Thrombosis: What It Is, How To Treat It And How To Prevent It
Non-Traumatic Intramural Hematomas In Patients On Anticoagulant Therapy
The New Oral Anticoagulants: Benefits, Dosages And Contraindications
Non-Traumatic Intramural Hematomas In Patients On Anticoagulant Therapy
Thrombus: Causes, Classification, Venous, Arterial And Systemic Thrombosis
Anticoagulant Drugs: List And Side Effects
Virchow’s Triad: The Three Risk Factors For Thrombosis


