Septic arthritis: symptoms, causes and treatment
Septic arthritis involves inflammation of a joint, the cause of which is to be found in colonisation by a pathogenic germ, usually a bacterium
The inflammation can lead to the formation of pus and, over time, also cause joint destruction, with considerable repercussions in terms of mobility.
The bacteria that cause inflammation are generally
- Staphylococcus Aureus (80% of cases),
- Haemophilus influenzae,
- Neisseria gonorrhoeae,
- Pseudomonas, especially in drug addicts and AIDS patients.
Depending on the number of joints affected by the bacterium one speaks of:
- monoarticular arthritis, if it involves a single joint (most cases);
- polyarticular form.
Symptoms of septic arthritis
The main symptoms are:
- limited movement
- pain that increases on digito-pressure;
- fever;
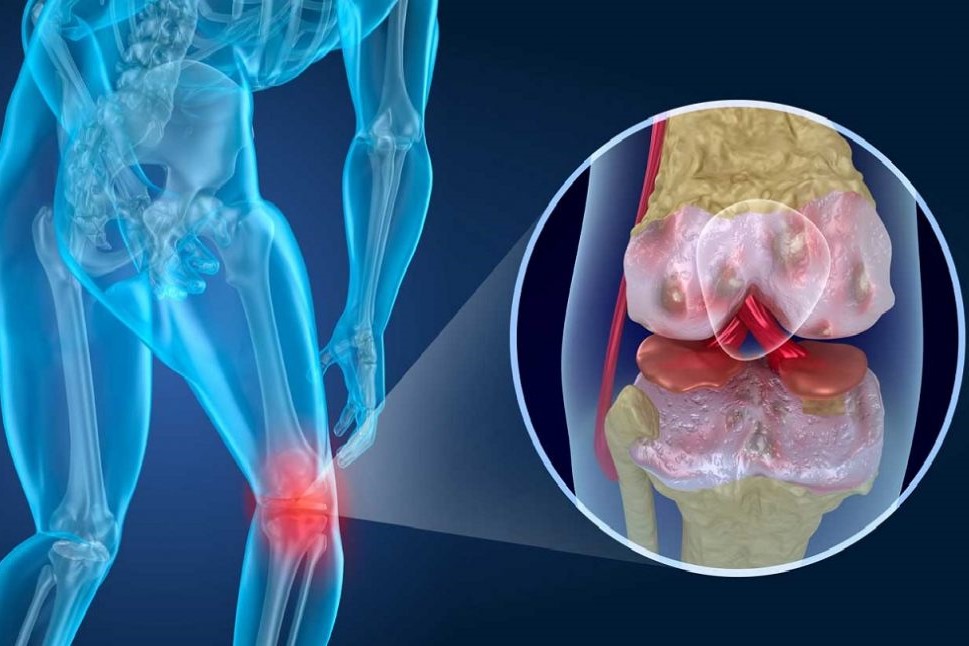
- swelling and reddening of the inflamed joint;
- joint abscesses.
The joints most affected are the larger, vascularised ones such as:
- shoulder;
- hip;
- knee;
- wrist;
- spine;
- ankle.
It is very rare for fungi (Candida) or viruses, e.g. hepatitis and rubella viruses, to affect the joints, causing septic arthritis.
The causes of septic arthritis
As mentioned above, the main agents responsible for septic arthritis can be:
- bacteria
- Staphylococcus Aureus;
- Haemophilus influenzae, often in unvaccinated children under 2 years of age;
- Pseudomonas aeruginosa, generally affected are drug addicts and AIDS patients or people with poor immune defences;
- Gonococcus, responsible for the typical form of gonococcal arthritis;
- Mycobacterium;
- Brucella (brucellar arthritis is a zoonosis, i.e. a disease contracted from infected animals);
- Treponema pallidum, responsible for syphilis;
- Borrelia burgdorferi, responsible for Lyme disease.
- viruses
- hepatitis B virus (HBV);
- rubella;
- mumps.
- fungi
- Candida albicans (micro-organism responsible for e.g. vaginal candida).
Risk factors
Very often septic arthritis is the consequence of previous joint diseases, whether spontaneous such as gout or not, such as rheumatoid arthritis.
But there are many other factors that can lead to the onset of septic arthritis, such as
- age, over 50-60 years;
- status of sepsis;
- diabetes and alcoholism;
- lowered immune defences due to diseases such as AIDS, neoplasms or use of immunosuppressants;
- drug addiction with intravenous drug use;
- joint surgery;
- systemic infectious diseases,
- exposed bone fractures.
Complications of septic arthritis can be quite serious and involve, for example, cartilage degeneration in the first 48 hours of infection, which can result in destruction of synovial tissue or distension of the joint capsule with pathological dislocation of joint bone segments.
Diagnosis of septic arthritis
It starts with a specific anamnesis, a clinical interview made by the specialist, which allows the patient’s recent and past clinical history to be reconstructed.
This is followed by an objective examination, where we try to understand the symptoms reported by the patient and often this test is enough to immediately diagnose the possible presence of infectious arthritis.
Blood tests show increased indices of inflammation, i.e:
- leucocytosis (increase in white blood cells),
- plateletosis (increase in platelets),
- increased ESR and C-reactive protein.
X-rays are one of the most frequently requested tests, although in the early stages of the disease the lesions may not be noticed.
Over time, signs of septic arthritis emerge, for example:
- distension of the capsule
- decreased joint space;
- inflammation of periarticular soft tissues;
- bone erosions.
- CT and MRI, on the other hand, are more incisive tests, useful in cases of arthritis affecting the spine, hips or knees.
Arthrocentesis is a surgical procedure that allows synovial fluid to be withdrawn with a syringe for diagnostic and therapeutic purposes.
Analysis of the synovial fluid helps the specialist to trace the aetiological agent responsible for the arthritis, and thus allows the prescription of more effective antibiotics.
How to treat septic arthritis
Generally, high-dose intravenous antibiotics are prescribed and this antibiotic therapy lasts from 6 weeks onwards.
The inflamed joint must be at rest and after 2-3 days of therapy, if there is an improvement, passive and finally active mobilisation of the joint can be started.
It may also be useful to drain the joint in order to remove any purulent material that has accumulated.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Arthrosis: What It Is And How To Treat It
Psoriatic Arthritis: How To Recognize It?
Arthrosis: What It Is And How To Treat It
Juvenile Idiopathic Arthritis: Study Of Oral Therapy With Tofacitinib By Gaslini Of Genoa
Rheumatic Diseases: Arthritis And Arthrosis, What Are The Differences?
Rheumatoid Arthritis: Symptoms, Diagnosis And Treatment
Joint Pain: Rheumatoid Arthritis Or Arthrosis?
The Barthel Index, An Indicator Of Autonomy
What Is Ankle Arthrosis? Causes, Risk Factors, Diagnosis And Treatment
Unicompartmental Prosthesis: The Answer To Gonarthrosis
Knee Arthrosis (Gonarthrosis): The Various Types Of ‘Customised’ Prosthesis
Symptoms, Diagnosis And Treatment Of Shoulder Arthrosis
Arthrosis Of The Hand: How It Occurs And What To Do
Arthritis: Definition, Diagnosis, Treatment, And Prognosis
Rheumatic Diseases: The Role Of Total Body MRI In Diagnosis
Rheumatology Tests: Arthroscopy And Other Joint Tests
Rheumatoid Arthritis: Advances In Diagnosis And Treatment
Diagnostic Tests: Arthro Magnetic Resonance Imaging (Arthro MRI)


