Shunt: what procedures are used
Shunt procedures are used to improve blood flow in the veins of the liver, oesophagus and other parts of the body, to stop bleeding, relieve pressure in these veins and relieve swelling
The porto-systemic shunt
Introduced in 1945, the portal (or porto-systemic) shunt was the first definitive form of therapy used for patients presenting with haemorrhage due to oesophageal varices.
The porto-systemic shunt involves surgically joining two veins, the portal vein and the inferior vena cava, in order to decrease the pressure in the portal vein (which carries blood to the liver).
The portal shunt is only performed in a relatively small number of patients, i.e. those with oesophageal variceal haemorrhage.
About a quarter of patients have such severe and uncontrollable haemorrhage that it can lead to death or the need for emergency surgery.
Patients eligible for portal shunt are those who are considered good candidates even for more demanding operations
The shunt virtually eliminates the bleeding caused by varicose veins, but its use as a technique declined in the 1970s for two main reasons.
One reason was the frequency with which encephalopathy presented itself as a complication.
The other was the failure of controlled clinical trials, carried out to establish whether there was a statistically significant advantage in the survival of patients treated with shunts over those treated with non-surgical therapy.
The failure of the portal shunt to improve survival reflected the associated complications of encephalopathy and post-shunt failure.
The distal spleno-renal shunt (DSRS)
This operation was created to preserve blood flow through the portal vein in the direction of the liver by decompressing the varices in the stomach and oesophagus through the spleen and splenic vein joined to the left kidney vein.
Studies comparing porto-systemic shunts with DSRS confirmed similar levels of mortality and survival.
DSRS had a higher mortality during the operation, but a lower risk of encephalopathy postoperatively.
Furthermore, patients with alcoholic cirrhosis did not find much benefit with DSRS compared to those with non-alcoholic cirrhosis.
The greatest merit of sclerotherapy is that it is relatively simple to perform and that it can also be administered in emergency departments.
Most physicians use a flexible endoscope to inject sclerosing solutions into oesophageal varices.
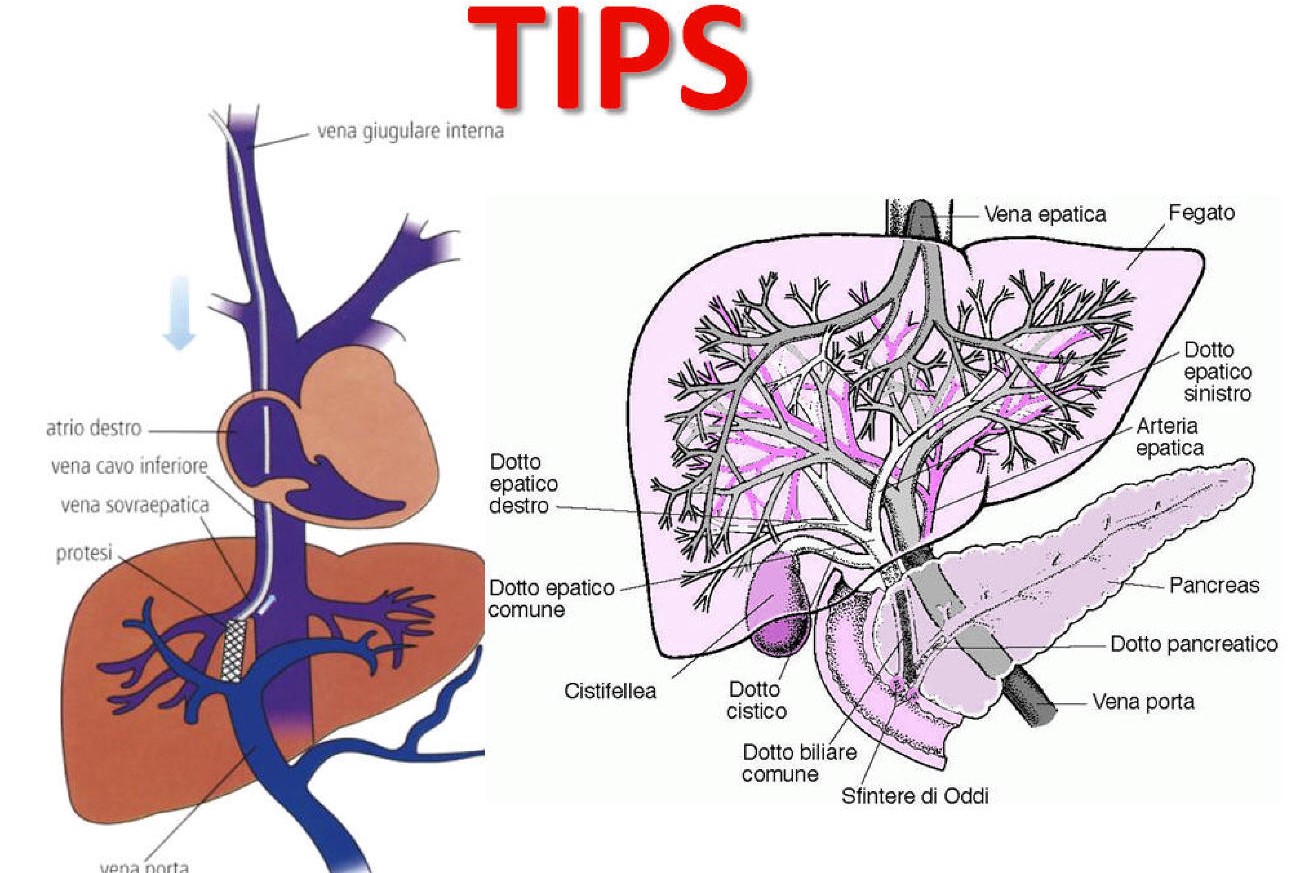
Transjugular intrahepatic porto-systemic shunt (TIPS)
An important recent benefit has been the development of the transjugular intrahepatic porto-systemic shunt (TIPS).
TIPS is performed by the radiologist, using only local anaesthesia and a sedative.
A long needle is inserted through the jugular vein in the neck, from there led to the hepatic vein and then into a branch of the portal vein in the liver.
Then the section between the portal vein branch and the hepatic vein is drained.
The major advantages of TIPS are that it does not require general anaesthesia or a more demanding surgical procedure, both of which are poorly tolerated by patients with cirrhosis.
In addition, TIPS reduces ascites (accumulation of fluid in the abdomen), unlike DSRS
It has indeed been successfully used to treat severe ascites (which no longer responded to diuretic drugs), to reduce fluid accumulation.
TIPS is a great innovation, but it is not without risks.
Although the direct mortality due to TIPS complications is relatively low (less than 5%), this is only true if the procedure is performed by experienced radiologists in specialised centres.
About a quarter of patients also develop encephalopathy after TIPS.
In a setting of lethal haemorrhage that no longer responds to sclerotherapy, TIPS is probably the ideal shunt procedure, if it is immediately available.
TIPS is not considered therapy of choice in patients with portal hypertension who do not respond to sclerotherapy and are candidates for liver transplantation.
This is because the presence of a surgical shunt makes transplantation more difficult, which may lead to a higher risk of complications and death after transplantation.
DSRS is preferable in a non-emergency surgery setting in patients who have recurrent haemorrhage despite sclerotherapy, but whose liver function is good.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Hepatitis In Children, Here Is What The Italian National Institute Of Health Says
Acute Hepatitis In Children, Maggiore (Bambino Gesù): ‘Jaundice A Wake-Up Call’
Nobel Prize For Medicine To Scientists Who Discovered Hepatitis C Virus
Hepatic Steatosis: What It Is And How To Prevent It
Acute Hepatitis And Kidney Injury Due To Energy Drink Consuption: Case Report
The Different Types Of Hepatitis: Prevention And Treatment
Acute Hepatitis And Kidney Injury Due To Energy Drink Consuption: Case Report
New York, Mount Sinai Researchers Publish Study On Liver Disease In World Trade Center Rescuers
Acute Hepatitis Cases In Children: Learning About Viral Hepatitis
Hepatic Steatosis: Causes And Treatment Of Fatty Liver
Hepatopathy: Non-Invasive Tests To Assess Liver Disease
Liver: What Is Non-Alcoholic Steatohepatitis
Hepatitis Outbreak In Children: 600+ Cases Worldwide, Cause Remains A Mystery
TIPS – Transjugular Porto-Systemic Shunt: What It Is, How It Works And When It Is Performed


