Stroke action first aid: actions to recognise and help
Stroke action first aid: A stroke occurs when blood flow in the brain is interrupted by a blockage or bleed in one of the blood vessels
This can cause damage to brain cells or cause them to die.
Blockages to the brain are a lot more common than bleeds.
Both have the same symptoms.
Strokes can happen to anyone of any age.
They are most common in older people, however, even babies can be victims of a stroke. Sadly for some people a stroke is fatal or can cause life-changing damage, yet some people are able to make a full recovery following a stroke.
THE RADIO OF THE WORLD’S RESCUERS? VISIT THE RADIO EMS BOOTH AT EMERGENCY EXPO
Stroke action first aid: What you are looking for?
Face – Can they smile and show their teeth?
Arms – Can they raise their arms and keep them held there, or does one arm fall?
Speech – Is their speech slurred? Can they repeat a phrase you give them? Do they have difficulty remembering words?
Time – If you see any of these three signs, it’s time to call Emergency Number.
TRAINING: VISIT THE BOOTH OF DMC DINAS MEDICAL CONSULTANTS IN EMERGENCY EXPO
Stroke, first aid: other potential symptoms
Sudden weakness or numbness on one side of the body, including legs, hands or feet
- Difficulty finding words or speaking in clear sentences
- Sudden blurred vision or loss of sight in one or both eyes
- Sudden memory loss or confusion, and dizziness; or a sudden fall.
- A sudden or severe headache
- Repeated vomiting
- Lack of balance
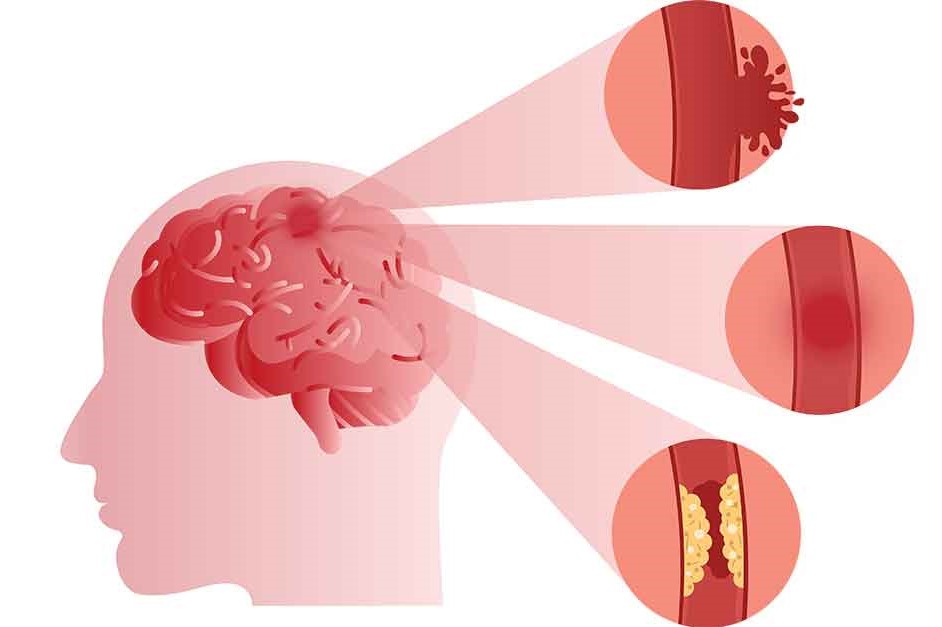
There are 2 main types of stroke: Caused by a blockage or a bleed
- Ischaemic – Which are caused by a blood clot blocking blood flow in the brain. These are more common and account for 85% of all cases. They can be caused by a build-up of plaque and fatty deposits in the arteries. If these plaques break away, or if they slow the blood flow to the extent that it forms a clot, they can block a blood vessel supplying the brain and cause a stroke.
- Haemorrhagic – Where a weakened blood vessel supplying the brain bursts
Trans-Ischaemic Attacks (mini-strokes)
A Trans-Ischaemic Attack (TIA) also known as a mini-stroke, is the same as a stroke, except that the symptoms last for a short amount of time, from just a few minutes to up to 24 hours.
TIAs are warning signs that someone is at high risk of having a stroke.
The FAST test can be used to recognise the signs of a TIA.
Any stroke-like symptoms should be taken seriously, and treated as a medical emergency.
Do not wait to see if symptoms get better. Early diagnosis and treatment can prevent a full stroke.
Rapid response is vital
Receiving medical attention as soon as possible after the stroke, decreases the amount of damaged caused.
If someone is showing the signs of a stroke, phone an ambulance immediately and get them to a specialist Stroke Unit as soon as possible.
Time is critical – an estimated 1.9 million neurons in the brain are lost every minute a stroke is untreated.
If the stroke is caused by a blood clot and they are able to receive clot-busting drug treatment (Alteplase) within four and a half hours, the symptoms of the stroke can be dramatically reduced.
Treating a stroke
Treatment depends on a number of factors.
You need to take into account your age, health and medical history, as well as the type of stroke you have had.
What caused the stroke and the area of the brain affected can determine different treatment.
Medication
Strokes are mostly treated with medication.
The medication would target reducing blood pressure, reducing cholesterol and preventing and dissolving blood clots.
Surgery
Sometimes, you can remove blood clots in surgery.
It is possible to perform a procedure similar to angioplasty in the heart, where blockages are removed by inserting a miniature wire into the blocked artery, removing the blockage and possibly inserting a stent to keep the vessel open and improve blood flow.
In the case of haemorrhagic strokes, surgery can also treat brain swelling and reduce the risk of further bleeding.
Recovering from a stroke
Those who survive a stroke can sustain an injury to their brain leaving them with long-term problems.
Some people make a good and swift recovery, for others it can be a very long and traumatic process.
Stroke is a leading cause of disability.
Almost two thirds of stroke survivors with a disability
Rehabilitation
In some cases a lengthy period of rehabilitation is needed before the person who has had a stroke can fully recover.
Although, the biggest steps in recovery are usually in the first few weeks after a stroke, the brain’s ability to ‘re-wire’ itself, known as neuroplasticity, means it is possible to continue to improve for months or years.
It can take a lot of effort and determination to keep going with rehabilitation.
It can be very hard work, physically and mentally, but many people find it helps them make vital progress with speaking, walking and other key skills.
Therapists work with you to set achievable goals. You can keep a record of your progress and celebrate your successes.
You might not be able to cope with much rehabilitation in the early days. When you feel stronger, you can do more.
Main risk factors for stroke:
Your age
The risk of suffering from a stroke increases as you get older.
This is due to the natural narrowing and hardening of our arteries as we age.
Strokes are most common in people over the age of 55.
Medical conditions
Certain medical conditions can increase your risk of stroke including:
- High blood pressure
- Diabetes
- Atrial fibrillation
- High cholesterol
An important way to reduce your risk of stroke is to find out if you have any of these conditions and work with your doctor to manage them.
Lifestyle factors
Lifestyle choices have a major impact on the risk of stroke.
Smoking, drinking too much alcohol, consuming too much salt, being overweight and eating unhealthy foods, damages blood vessels, increases blood pressure and dramatically raises the risk of stroke.
Conversely, changing lifestyle and making healthy choices to reduce the stress to blood vessels can substantially reduce the likelihood of someone experiencing a stroke.
Some ethnicities are at higher risk of stroke
People with African, Caribbean or South Asian backgrounds have a higher predisposition to diabetes, atherosclerosis and high blood pressure.
These underlying medical conditions greatly increase the risk of stroke.
Link with the contraceptive pill
Overall, the risk of stroke from using contraception is low but some types of hormone-based contraception do carry an increased risk of stroke.
However, check your risk of stroke carefully before you are given any of these treatments by the doctor.
Women with risk factors for stroke may not be able to use contraceptive pills containing oestrogen.
This is because high levels of the female hormone oestrogen can make your blood more likely to clot.
However, if you are concerned about using the pill, or you want to find out more about your risk of a stroke, speak to your GP.
Pregnant women
Health conditions that can affect pregnant women such as pre-eclampsia and gestational diabetes can raise your risk of a stroke.
However, routine ante-natal checks should pick up and treat these issues if they occur.
Furthermore, if you have any health concerns when pregnant, always speak to your midwife or GP immediately.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Stroke-Related Emergencies: The Quick Guide
Emergency Stroke Management: Intervention On The Patient
Ischaemia: What It Is And Why It Causes A Stroke
How Does A Stroke Manifest Itself? Signs To Watch Out For
Treatment Of Urgent Stroke: Changing Guidelines? Interesting Study In The Lancet
Benedikt Syndrome: Causes, Symptoms, Diagnosis And Treatment Of This Stroke
What Is A Positive Cincinnati Prehospital Stroke Scale (CPSS)?
Foreign Accent Syndrome (FAS): The Consequences Of A Stroke Or Severe Head Trauma
Acute Stroke Patient: Cerebrovascular Assessment
Basic Airway Assessment: An Overview
Three Everyday Practices To Keep Your Ventilator Patients Safe
Benefits And Risks Of Prehospital Drug Assisted Airway Management (DAAM)
Respiratory Distress Syndrome (ARDS): Therapy, Mechanical Ventilation, Monitoring
Chest Pain, Emergency Patient Management
Ambulance: What Is An Emergency Aspirator And When Should It Be Used?
Notions Of First Aid: The 3 Symptoms Of A Pulmonary Embolism
Quick And Dirty Guide To Chest Trauma
Neonatal Respiratory Distress: Factors To Take Into Account
Resuscitation Manoeuvres: Cardiac Massage On Children
Emergency-Urgency Interventions: Management Of Labor Complications
What Is Transient Tachypnoea Of The Newborn, Or Neonatal Wet Lung Syndrome?
Tachypnoea: Meaning And Pathologies Associated With Increased Frequency Of Respiratory Acts
Postpartum Depression: How To Recognise The First Symptoms And Overcome It
Postpartum Psychosis: Knowing It To Know How To Deal With It
Clinical Review: Acute Respiratory Distress Syndrome
Seizures In The Neonate: An Emergency That Needs To Be Addressed
Stress And Distress During Pregnancy: How To Protect Both Mother And Child
Respiratory Distress: What Are The Signs Of Respiratory Distress In Newborns?
Respiratory Distress Syndrome (ARDS): Therapy, Mechanical Ventilation, Monitoring
Childbirth And Emergency: Postpartum Complications
Signs Of Respiratory Distress In Children: Basics For Parents, Nannies And Teachers
Three Everyday Practices To Keep Your Ventilator Patients Safe
Ambulance: What Is An Emergency Aspirator And When Should It Be Used?
The Purpose Of Suctioning Patients During Sedation
Supplemental Oxygen: Cylinders And Ventilation Supports In The USA
Behavioural And Psychiatric Disorders: How To Intervene In First Aid And Emergencies
Fainting, How To Manage The Emergency Related To Loss Of Consciousness
Altered Level Of Consciousness Emergencies (ALOC): What To Do?
Respiratory Distress Emergencies: Patient Management And Stabilisation


