Tachycardia: let's talk about heart rate
When, in a resting condition, there is an increase in heart rate above values considered normal, we speak of tachycardia
This condition is due to an abnormality in the generation or propagation of the electrical impulses that control cardiac contraction and can be of a different nature, depending on the site from which the impulse starts.
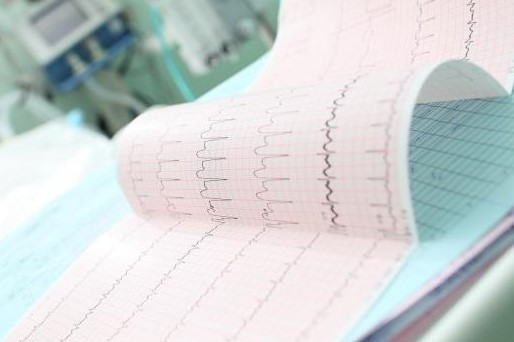
Diagnosis of this disorder requires an electrocardiogram (ECG), which records the heart’s electrical impulses and their conduction, while treatment may vary depending on the specific cause.
What is tachycardia
Normally, in resting conditions, the heart rate is between 60 and 100 beats per minute; therefore, we speak of tachycardia whenever the resting heart rate (HR) exceeds 100 beats per minute (bpm).
The nature and causes of the disorder can be of different origins, and the diagnosis of these conditions involves certain specific investigations.
Heart rate is finely regulated by a series of mechanisms that affect the way electrical impulses are transmitted to the muscle through the cardiac tissue; under certain circumstances, abnormalities may occur in the heart’s electrical networks and thus the rate may rise or fall excessively, causing episodes of tachycardia or brachycardia, respectively.
Although in some cases, such as stress, trauma or fever, tachycardia is not related to other health problems, it can be an important warning sign that should not be underestimated: it may be an indication of heart disease or other underlying pathological conditions.
Types of tachycardia
How the heart’s electrical networks work
In the heart, inside the right atrium, there is the so-called sinoatrial node, a kind of natural pacemaker from which electrical impulses originate; these impulses are transmitted to the muscle tissue of the atria, triggering contraction and the resulting blood circulation.
The electrical signals then reach the so-called atrioventricular node, which transmits them to another group of cells, called the His bundle, which in turn conducts the impulse from the atrioventricular node to the two ventricles, which contract, pumping blood into the body.
Paroxysmal or sinus tachycardia and other heart rate disorders
Clinically, there are two different types of tachycardia: paroxysmal tachycardia and sinus tachycardia.
There are also other types of heart rhythm disorders that can cause tachycardia.
The most frequent manifestation of the pathologies belonging to the first group is paroxysmal supraventricular tachycardia (TPSV): this is an arrhythmia due to the abnormal generation of the electrical impulse, which starts from a point other than the sinoatrial node, altering the heart rhythm for a longer or shorter period of time.
In such cases, the heart rate can reach over 200 beats per minute and attacks may be accompanied by anxiety, sweating, hypotension and heart palpitation (palpitations).
The causes of arrhythmia can be many, ranging from cardiac lesions and congenital defects to drug intoxication or gastrocardiac reflexes.
Given the paroxysmal nature of these arrhythmias, attacks tend to occur and die out suddenly and can affect even the very young.
In the second case, however, sinus tachycardia is a much more common and less dangerous form of arrhythmia: it is caused by an increase in sinus rhythm (i.e. generated correctly by the atrial sinus node).
It is usually triggered by physiological causes such as strong emotions or excitant substance abuse, and episodes tend to occur gradually.
Among the most common disorders that can lead to the onset of tachycardia are:
- Atrial fibrillation: this is a condition in which electrical impulses are generated in a disordered and irregular manner, causing accelerated and uncoordinated contraction of the atria. Atrial fibrillation is the most common type of condition that can lead to tachycardia and can occur with advancing age or in individuals with cardiovascular or cardiopulmonary diseases.
- Atrial flutter: The symptoms and causes of atrial flutter are very similar to those of atrial fibrillation, however this condition differs in that the atria contract rhythmically although at much higher frequencies than normal. It is a less common disorder, often associated with other pathologies; atrial flutter attacks may resolve on their own or require specific therapy.
- Ventricular fibrillation: in this condition, the ventricles contract in a disordered manner, failing to pump blood effectively into the circulation; it is a serious disorder that can have very severe complications and even lead to death within minutes if action is not taken promptly to resolve the arrhythmia. Most people who suffer from ventricular fibrillation generally have other heart diseases or have suffered a myocardial infarction.
Possible causes of tachycardia
If abnormalities occur in the heart’s electrical system, more or less severe arrhythmias may appear, which may manifest as tachycardia.
There are certain conditions that can physiologically lead to the onset of this condition, due to the increased metabolic needs of the tissues.
These include intense physical activity, situations of stress or anxiety, and illnesses that lead to an increase in body temperature.
Some behaviours are related to temporary alterations in heart rate, such as smoking, alcohol consumption or the intake of exciting substances such as caffeine.
Finally, there are pathological causes and medications that can interfere with the normal electrical activity of the heart; these include:
- Thyroid overactivity (hyperthyroidism);
- Hypertension or arterial hypotension;
- Anaemia;
- Heart disease, endocarditis or myocarditis;
- Congenital malformations;
- Tumours;
- Damage to cardiac muscle tissue that may be caused by cardiovascular disease or trauma, such as a myocardial infarction;
- Electrolyte imbalance, due to the excess or lack of certain mineral substances necessary for the correct generation of electrical impulses;
- Infections or sepsis;
- Acute inflammation;
- Cardio-respiratory diseases;
Symptoms and complications
During tachycardia, the heart beats too fast, disrupting the correct sequence of contractions and relaxations necessary for blood to be adequately pumped to all bodily districts; on the one hand, this results in certain tissues being poorly supplied with blood, leading to certain symptoms often associated with tachycardia conditions, i.e. difficulty breathing, palpitations, fainting, chest pain and dizziness; on the other hand, it places the heart muscle under stress, requiring more blood, oxygen and nutrients.
Diagnosis
When the patient shows symptoms attributable to tachycardia conditions, the most suitable procedure for diagnosing this disorder is the electrocardiogram: the ECG is a completely safe and non-invasive diagnostic test, which involves the use of a series of electrodes attached to the patient’s chest and arms, which record the heart’s electrical activity, transmitting them to a screen in the form of a trace for reading.
There are three types of electrocardiogram: the resting ECG, the dynamic ECG, which records cardiac activity for a prolonged time, and the exercise ECG.
In cases where the tachycardia is intermittent and is not detected with the classic ECG, a cardiac Holter (or dynamic ECG according to Holter) may be prescribed, in which the heartbeat is monitored for at least 24 hours using portable devices.
Further investigations such as an echocadiogram, i.e. an ultrasound scan of the heart in motion, which can detect changes in heart muscle function, areas of poor blood circulation and abnormal valves; or a tilt-test, i.e. a passive orthostatic stimulation test, can be used for diagnostic purposes.
Treatment
Some forms of tachycardia do not require any treatment, while in other cases it is necessary to intervene with drug therapy.
In addition to slowing the heartbeat during the attack, treatment should aim to prevent future episodes and reduce the risk of complications.
In particular, the cardiologist can prescribe anti-arrhythmic drugs, calcium channel blockers and beta-blockers to regularise the heart rate.
Alternatively, for less severe cases and on the advice of your doctor, you can perform certain manoeuvres to lower your heart rate: these include forced exhalation with the glottis closed (Valsalva manoeuvre), applying ice to the face, unilateral compression of the carotid artery or bilateral massage of the eyeballs.
These procedures should be performed under strict medical supervision, as they can lead to significant side effects.
In more severe cases, more invasive procedures may be necessary, such as cardiac ablation, which involves inserting small leads into the blood vessels in order to destroy the area where the abnormal impulses are generated.
Other forms of tachycardia can be treated with the insertion of a pace-maker or implantable cardioverter defibrillator (ICD), pulse-generating devices that are implanted in the chest and regulate the heart rate appropriately.
Finally, in emergency conditions, cardioversion, a procedure in which the heart is stimulated by electrical impulses via an automatic external defibrillator (AED), can be used.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Syncope: Symptoms, Diagnosis And Treatment
Head Up Tilt Test, How The Test That Investigates The Causes Of Vagal Syncope Works
Cardiac Syncope: What It Is, How It Is Diagnosed And Who It Affects
New Epilepsy Warning Device Could Save Thousands Of Lives
Understanding Seizures And Epilepsy
First Aid And Epilepsy: How To Recognise A Seizure And Help A Patient
Neurology, Difference Between Epilepsy And Syncope
First Aid And Emergency Interventions: Syncope
Epilepsy Surgery: Routes To Remove Or Isolate Brain Areas Responsible For Seizures
Heart Pacemaker: How Does It Work?
Paediatric Pacemaker: Functions And Peculiarities
What Is The Difference Between Pacemaker And Subcutaneous Defibrillator?
Heart: What Is Brugada Syndrome And What Are The Symptoms
Diagnosis Of Mitral Stenosis? Here’s What’s Happening
Genetic Heart Disease: Brugada Syndrome
Cardiac Arrest Defeated By A Software? Brugada Syndrome Is Near To An End
Heart: Brugada Syndrome And The Risk Of Arrhythmia
Heart Disease: First Study On Brugada Syndrome In Children Under 12 From Italy
Mitral Insufficiency: What It Is And How To Treat It
Semeiotics Of The Heart: History In The Complete Cardiac Physical Examination
Electrical Cardioversion: What It Is, When It Saves A Life
Heart Murmur: What Is It And What Are The Symptoms?
Performing The Cardiovascular Objective Examination: The Guide
Branch Block: The Causes And Consequences To Take Into Account
Cardiopulmonary Resuscitation Manoeuvres: Management Of The LUCAS Chest Compressor
Supraventricular Tachycardia: Definition, Diagnosis, Treatment, And Prognosis
Identifying Tachycardias: What It Is, What It Causes And How To Intervene On A Tachycardia
Myocardial Infarction: Causes, Symptoms, Diagnosis And Treatment
Aortic Insufficiency: Causes, Symptoms, Diagnosis And Treatment Of Aortic Regurgitation
Congenital Heart Disease: What Is Aortic Bicuspidia?
Atrial Fibrillation: Definition, Causes, Symptoms, Diagnosis And Treatment
Ventricular Fibrillation Is One Of The Most Serious Cardiac Arrhythmias: Let’s Find Out About It
Atrial Flutter: Definition, Causes, Symptoms, Diagnosis And Treatment
What Is Echocolordoppler Of The Supra-Aortic Trunks (Carotids)?
What Is The Loop Recorder? Discovering Home Telemetry
Cardiac Holter, The Characteristics Of The 24-Hour Electrocardiogram
Peripheral Arteriopathy: Symptoms And Diagnosis
Endocavitary Electrophysiological Study: What Does This Examination Consist Of?
Cardiac Catheterisation, What Is This Examination?
Echo Doppler: What It Is And What It Is For
Transesophageal Echocardiogram: What Does It Consist Of?
Paediatric Echocardiogram: Definition And Use
Heart Diseases And Alarm Bells: Angina Pectoris
Fakes That Are Close To Our Hearts: Heart Disease And False Myths
Sleep Apnoea And Cardiovascular Disease: Correlation Between Sleep And Heart
Myocardiopathy: What Is It And How To Treat It?
Venous Thrombosis: From Symptoms To New Drugs
Cyanogenic Congenital Heart Disease: Transposition Of The Great Arteries
Heart Rate: What Is Bradycardia?
Consequences Of Chest Trauma: Focus On Cardiac Contusion


