Thalassaemia or Mediterranean anaemia: what is it?
The term thalassaemia (Mediterranean anaemia or microcytic anaemia) defines a heterogeneous group of hereditary anaemias, caused by an alteration in the genes that regulate haemoglobin production
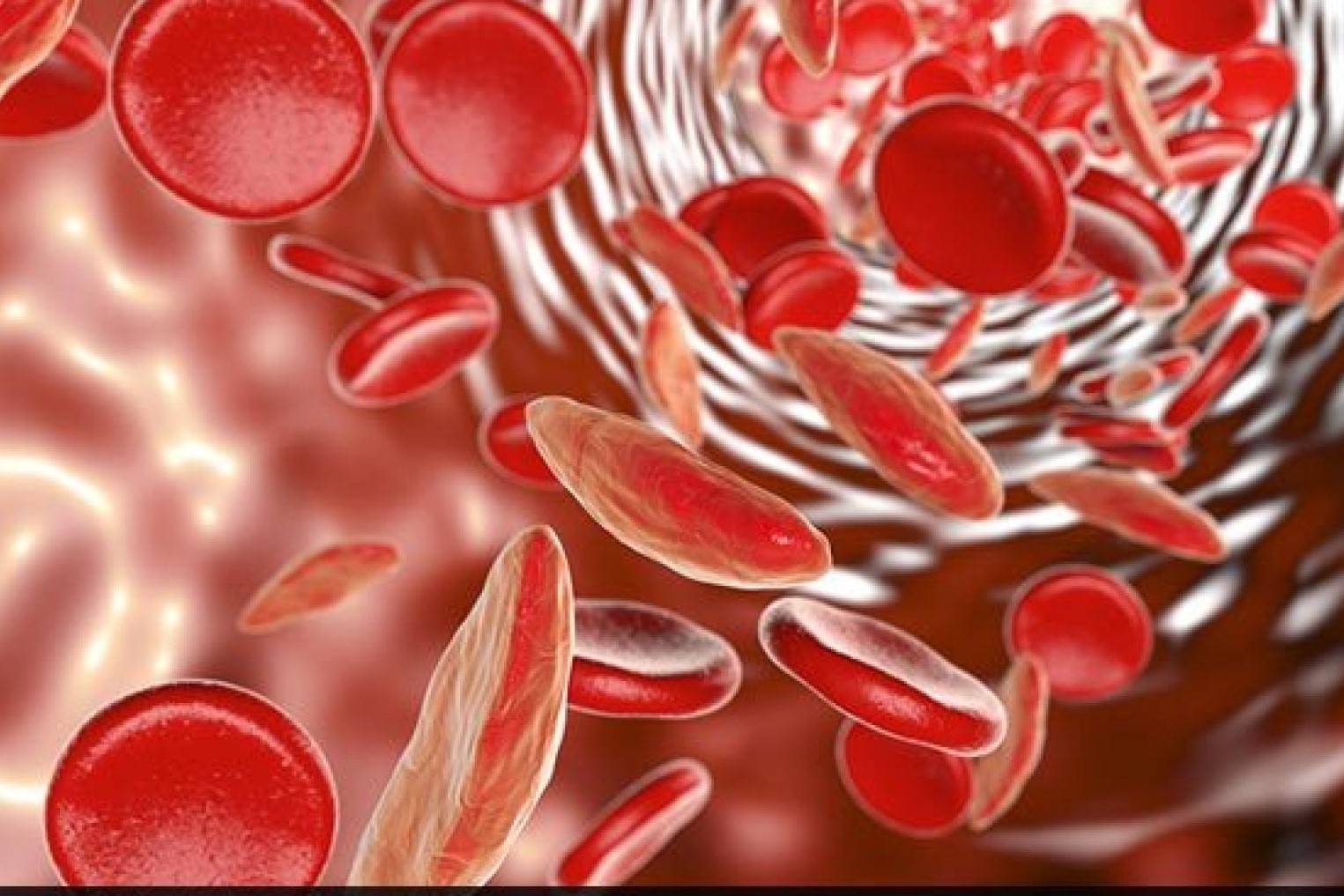
Haemoglobin is a protein, contained in red blood cells, whose function is to transport oxygen to the body’s cells and to eliminate carbon dioxide.
In thalassaemia, the lack of production of normal haemoglobin leads to early destruction of red blood cells
Thalassaemia is a widespread hereditary disease worldwide, affecting more than 20% of the population in some areas.
In Italy, the number of healthy carriers is about 2,000,000, while thalassaemia patients number about 7,000.
Thalassaemia: how to tell if you are a healthy carrier
Being a healthy carrier means that one of the two genes that control the production of haemoglobin is defective, but because the other gene works well, the carrier is a healthy person.
The status of a healthy thalassaemia carrier can be identified by performing first-level haematological examinations (screening for thalassaemia), carried out in qualified centres.
In particular:
- blood count;
- Hb A2 dosage;
- Hb F dosage;
- research of abnormal haemoglobins;
- osmotic resistance;
- sideremia;
- ferritinemia;
Inheritance of thalassaemia
When a child is conceived it receives genes from each of its two parents; if they are both thalassaemia carriers (risk couple), it may receive either the normal or the defective gene from each of them:
- if the child receives the normal genes it will be normal (little white man; 25% probability);
- if he receives one normal and one defective gene he will be a healthy carrier, like his parents (little man half red and half white; 50% probability);
- if he receives both defective genes he will have thalassaemia because he will not be able to produce normal haemoglobin for his red blood cells (little red man, 25% probability).
- It is therefore important for everyone to take screening tests to find out if they are a healthy carrier of thalassaemia.
If two carriers decide to have a child, they must undergo level II investigations:
- DNA extraction;
- DNA mutation analysis.
These examinations are essential to identify the type of molecular defect, on the basis of which, after genetic counselling, an indication is given for prenatal diagnosis, which is carried out between the 10th and 12th week of gestation, with examination of the foetal DNA extracted from the chorionic villi.
Thalassaemia Major and Minor
Thalassaemia minor – thalassaemia trait carrier or healthy thalassaemia carrier – defines the status of a thalassaemia carrier.
It is present in a subject who has an alteration in one of the two genes responsible for haemoglobin synthesis.
The subject is asymptomatic, may show a slight reduction in haemoglobin concentration, a smaller red blood cell than normal and requires no treatment.
Thalassaemia major is a disease that occurs in a patient when there is an alteration in both genes responsible for haemoglobin synthesis.
The first signs of the disease generally appear in the first year of life.
The child shows growth problems, slight bone deformities, an increase in the volume of the liver and spleen, and anaemia.
It is necessary to give him or her a concentrated blood transfusion to ensure a ‘normal’ life.
The child is periodically given blood transfusions, but over time these lead to an accumulation of iron in the body.
The accumulated iron can give problems
- cardiac (cardiomyopathy, heart failure, arrhythmias);
- hepatic (fibrosis, cirrhosis, hepatocarcinoma);
- endocrine (lack of pubertal development, hypothyroidism, diabetes, hypoparathyroidism).
They can be avoided by taking medication that promotes iron elimination.
Thalassaemia therapy
Bone marrow transplantation was the first form of therapy that can lead to a definitive cure for people with thalassaemia major.
However, this intervention is possible when a compatible consanguineous donor (brother or sister) is available, or when a compatible non-consanguineous donor is available among those registered in the international bone marrow donor bank.
Bone marrow transplantation carries a low risk of rejection or death.
Future prospects are based on the possibility of using new oral iron chelators, including a new molecule that can be taken very easily, and on gene therapy, which may make it possible to transplant genetically ‘corrected’ stem cells capable of producing normal haemoglobin into thalassaemic patients.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Mediterranean Anaemia: Diagnosis With A Blood Test
Iron Deficiency Anaemia: What Foods Are Recommended
What Is Albumin And Why Is The Test Performed To Quantify Blood Albumin Values?
What Is Cholesterol And Why Is It Tested To Quantify The Level Of (Total) Cholesterol In The Blood?
Gestational Diabetes, What It Is And How To Deal With It
What Is Amylase And Why Is The Test Performed To Measure The Amount Of Amylase In The Blood?
Adverse Drug Reactions: What They Are And How To Manage Adverse Effects
Albumin Replacement In Patients With Severe Sepsis Or Septic Shock
Provocation Tests In Medicine: What Are They, What Are They For, How Do They Take Place?
What Are Cold Agglutinins And Why Is The Test Performed To Quantify Their Values In The Blood?


