Tuberculosis, symptoms and transmission
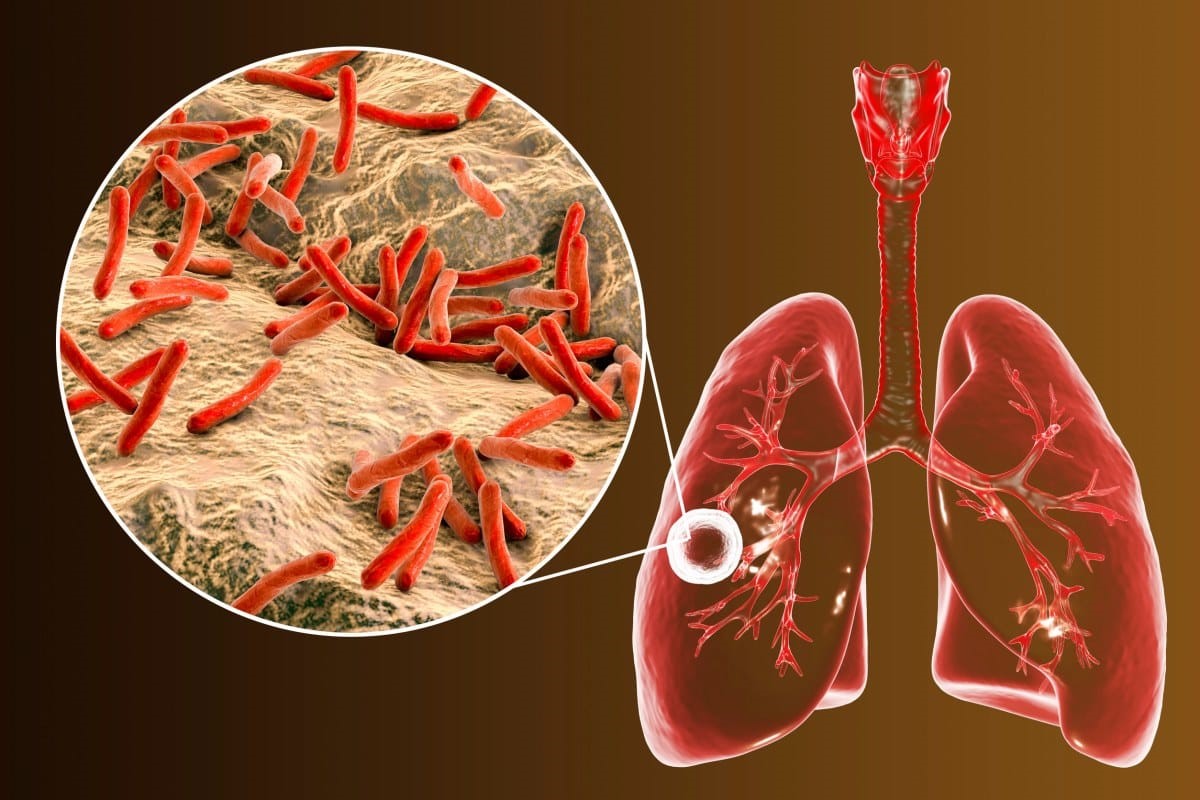
Tuberculosis is a lung infection caused by a bacterium, Mycobacterium tuberculosis. The bacterium that causes Tuberculosis (TB) is spread from one person to another when you come into contact with the cough or sneeze of someone who is already infected
It is enough to inhale a small amount of germs to be infected.
Tuberculosis develops in patients in whom the immune system has failed to block the primary infection, and occurs a few weeks after this
The first consequence of the infection is the production of granulomas in the infected tissue.
In this first stage of the disease, usually called the ‘primary stage’, the patient does not yet present the symptoms of the disease (cough, phlegm, blood in the sputum and chest pain).
Those most at risk are the elderly, children and individuals with a weakened immune system: transplant recipients, cancer patients undergoing chemotherapy or HIV patients.
Typical symptoms of tuberculosis are:
- coughing with phlegm and presence of blood;
- chest pain;
- weakness and tiredness;
- loss of weight and appetite;
- fever and night sweats.
These may be associated with other symptoms such as dyspnoea, difficulty breathing and wheezing.
Tuberculosis and contagion: how is TB transmitted?
Tuberculosis is present in every part of the world, however, the most affected areas are Asia (61% of new cases per year) and Africa (26% of new cases per year).
In 2015, 87% of new TB cases occurred in poorer countries such as India, Indonesia, China, Nigeria, Pakistan and South Africa.
TB is transmitted by air contact (through coughs and sneezes) with infected patients, but not through personal belongings: clothes, bed or any object that is touched by infected people.
In order for the disease to be transmitted, exposure to the bacteria must be prolonged, both during the day and over time, as there are very few micro-organisms contained in the coughs or sneezes of infected persons.
It should be remembered that only patients with active tuberculosis are contagious, i.e. those in whom the disease has fully manifested itself.
Latent tuberculosis
About one third of the world’s population contracts tuberculosis latently.
This means that one can be infected with the tuberculosis bacterium without developing the disease.
In the case of latent Tuberculosis, the person is not able to transmit the Tuberculosis bacterium, but is 10% more likely to develop the disease.
Course of TB
The infection begins in the alveoli, where macrophages attack the bacterium.
Some bacilli are killed immediately, while others multiply within the macrophages themselves.
During the first stage of the disease, in people with a good immune system, the macrophages present fragments of the bacilli on their surface so that the T-cells, stimulated by this situation, release chemical signals. At this stage, the patient is positive in the tuberculin test, which establishes the infection.
Many patients do not go beyond the first stage of the disease and the tuberculin test can only ascertain that they are infected.
Diagnosis and complications of Turbeculosis
The doctor’s first approach is undoubtedly auscultation of the chest, which usually reveals the presence of rales; enlarged lymph nodes may also be present in the neck area.
The diagnosis of tuberculosis can sometimes be difficult as this disease tends to resemble, or even present together with, other respiratory diseases such as pneumonia, tumours, lung abscesses or fungal infections.
In making the diagnosis, the specialist will take into account the symptoms and other tests to detect the presence of the tuberculosis bacterium, such as
- mucus culture
- bronchoscopy
- chest X-ray
- the tuberculin test.
If diagnosed late or inadequately treated, tuberculosis can cause permanent damage to the lungs and in the worst cases can be fatal.
Anti-tuberculosis drugs can also cause damage; more specifically, some of them can induce non-viral hepatitis, others give a dark or orange colouration to tears and urine, and others cause reduced visual acuity.
Tuberculin test: what it is and how it is performed
This is a skin test in which antigen is administered to the patient by injecting it under the skin of the arm to see if there has been exposure to the tuberculosis bacterium.
After about 48-72 hours, if the test is positive, the skin will show red and swollen, as if an allergy was present or the patient had been bitten by an insect.
If the test is negative, the skin may be red, but not swollen.
No special preparation is needed to perform the test; the only caution concerns people suffering from dermatitis or other skin irritations, which could easily be mistaken for a positive test result.
There is no risk for the patient as the amount of antigen injected is very minimal; however, one might feel a slight itching in the area of the injection.
One last consideration should be borne in mind: there may be false positives in immunodepressed persons, such as transplant patients, cancer patients undergoing chemotherapy treatment or AIDS patients, and in persons taking large amounts of steroids.
Treatment: how to treat TB
Treatment is essentially based on curing the infection by administering anti-tuberculosis drugs.
Treatment goes on for at least six months, but may continue beyond that if the response to treatment is not as good as expected.
The prognosis is excellent if tuberculosis is diagnosed and treated in time and adequately, and symptoms improve in about 3 weeks.
A healthy lifestyle can also help to recover quickly from the disease; it is important, for example, to always take the prescribed medication, scrupulously following the manner and timing of its administration, to avoid anything that may compromise the immune system, such as alcohol, to eat a balanced diet based on fruit and vegetables, and to get plenty of rest.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Who Gets Tuberculosis? Harvard Medical School Study On Immune Cell Deficiency
Médecins Sans Frontières MSF, New Strategies At Work In Eleventh Ebola Outbreak In DRC
MSF: Lifesaving TB (Tubercolosis) Medicines Still Out Of Reach For Children In High-Burden Countries


