Uterine fibroid embolization: what it is and how to treat it
Arterial embolization, the most brilliant therapeutic solution at the end of the last century respecting the woman’s ‘self image’, is the alternative to surgery for symptomatic uterine fibroids
Developed in France by Prof. Ravinà, a gynaecologist, and Prof. Merland, an interventional radiologist, embolisation has been practised in Paris since 1993, in the United States of America since 1995, in England, Israel and Canada since 1997, and in Italy, first and foremost in Brescia, since May 1997.
Embolization of uterine fibroids, to date some 2000 operations have been performed worldwide
Previously reserved only for women between the ages of 38 and 48 who no longer had the desire to become pregnant, the indication has now been extended to young women who wish to preserve their fertility.
Uterine fibroma
Uterine fibroids affect about 35% of women of childbearing age, although only in 50% of cases do they become symptomatic.
However, they are the most frequent pelvic tumours.
This disease is hormone-dependent; fibroid formation is linked to high circulating oestrogen rates.
In fact, after the menopause, as oestrogen falls, fibroids tend to spontaneously regress.
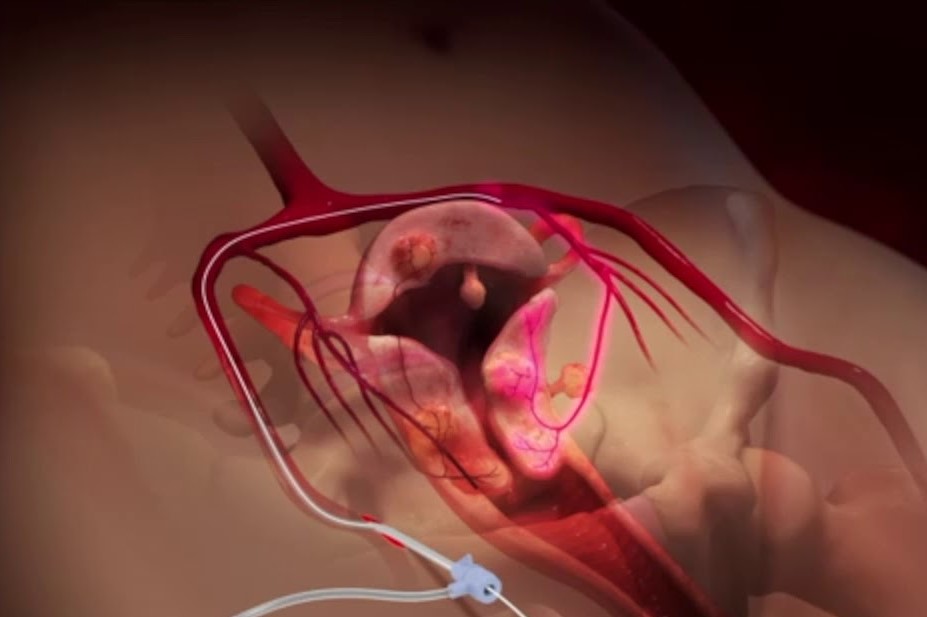
The body of the uterus is supplied by uterine arteries that branch off in short branches; in the presence of fibroids, the uterine artery increases in calibre and the vascularisation of the fibroid is greater than that of the surrounding myometrium.
The vascularisation of fibroids consists of a peripheral network and a centripetal network.
The first, the most important, surrounds the tumour and is formed by capillary and fibromatous vessels anastomosed with uterine arteries.
This peritumoral vascular network is responsible for bleeding during myomectomy.
The second, more slender, is composed of multiple branches, which reduce distally to a few terminal arterioles.
This vascularisation of the fibroids is low resistance and accounts for the selective distribution of microparticles during embolisation.
The symptoms of uterine fibroids are variable: menometrorrhagia, compression of the neighbouring pelvic viscera, infertility from mechanical causes
Menometrorrhagia are the most important symptom of submucosal and interstitial fibroids, and are more abundant in the perimenopausal period due to relative hyperestrogenism.
Such menometrorrhagia are traced back to endometrial hyperplasia and increased uterine cavity, however peritumoral hypervascularisation probably plays a greater role.
Today, there is no aetiological or preventive treatment, and only symptomatic uterine fibroids require treatment.
There are hormonal and surgical therapies.
Arterial embolization
Arterial embolisation has been used for many years in obstetrics and gynaecology.
As early as 1980, embolisation of the hypogastric arteries was shown to be the ultimate treatment of irrepressible haemorrhage during secondment.
Subsequently, temporary embolisation of uterine arteries was used before complex myomectomies in order to reduce perioperative bleeding and facilitate the surgical act.
Between 1989 and 1993, embolisation was used in 6 women with symptomatic uterine fibroids with associated pathology (obesity, previous thromboembolic episodes, AIDS, brain tumour) involving a high operative risk.
It was subsequently proposed as an alternative treatment to fibroid surgery.
The multicentre study conducted by Prof. Ravinà and Prof. Merland allowed the creation of guidelines on arterial embolization of uterine fibroids
Inclusion criteria presence of a fibromatous uterus with symptomatic fibroids, identified clinically and ultrasoundologically, that are not pedunculated; persistent haemorrhagic and compressive symptoms, despite well-conducted medical treatment, or symptoms that threaten the woman’s physical integrity (serious haemorrhages); absence of hormonal treatment for at least 3 months (the cause of 3 of the 5 failures reported in the literature); presence of a high anaesthesiological and operative risk, contraindicating surgery; adherence to follow-up.
Exclusion criteria: presence of non-symptomatic uterine fibroids; menometrorrhagia related to malignant pathologies; women on hormonal treatment with progestins and/or GnRh analogues; women who cannot ensure adequate follow-up; contraindications to arteriography (arterial prostheses, ischaemic risk); allergy to iodine products; allergic diathesis; patient refusal.
Pre-operative care in uterine fibroid embolization
Patients are assessed in consultation by the gynaecologist (for a clinical and instrumental assessment to exclude other causes of menometrorrhagia and to estimate their extent: blood count, sideremia, ferritinemia, pap smear, pelvic ultrasound); by the anaesthetist (for preoperative assessment); by the interventional radiologist (to inform the patient about the technique).
The patient will be given an information note and asked to sign an informed consent.
After discussion of the clinical case and collegial agreement, the patient will be admitted the day before the operation, with blood chemistry and instrumental examinations (blood group, blood count, Quick time, PT, PTT, bleeding time, CPK, etc.).
The patient will be fasting from midnight and will go to the radiology room with a peripheral venous access.
Intervention technique
The procedure takes place in a state-of-the-art angiography room with an arcus for interventional radiology.
The embolisation materials are the classic ones used for an arterial catheterisation with the added need for a microcatheter, Tracker type, and microparticles (inert polyvinylformaldehyde).
After local anaesthesia, the femoral artery is cannulated and selective catheterisation of the ipsilateral or more often contralateral hypogastric artery is performed to map the tumour vasculature.
Then, the uterine artery is selectively catheterised while remaining proximal to avoid arterial vasospasm that would prevent microparticle progression; the microcatheter is then placed.
Selective embolisation is performed with free flow so that the microparticles can occlude the peritumoral vascular bed.
Once the probe is placed in the uterine artery, embolization can begin
The injection of microparticles into the peritumoral vascular bed is stopped when stagnation appears.
This manoeuvre is also performed contralaterally. In fact, even if there is only unilateral hypervascularisation, there is a risk of failure for contralateral restoration of the tumour vasculature.
After ensuring successful devascularisation, the catheter and introducer are removed.
A compression dressing is placed over the entry point and the patient is taken back to the ward.
The procedure lasts approximately one hour.
A general aortography is rarely necessary; instead, it is optimal to perform an opacification of each uterine artery before and after embolisation.
Postoperative care
After embolisation, the occurrence of pelvic pain depends on the volume of the fibroids.
The pain may be immediate and last 12-18 hours, followed for a few days by soreness, probably of ischaemic origin.
This requires appropriate analgesic treatment: from morphine-like venous infusions via a self-administered pump, to non-steroidal anti-inflammatory drugs for a week, from antispasmodics to antinausea.
In cases of large fibroids, epidural anaesthesia is useful.
When fibroids are 10-12 cm in diameter, a delayed symptomatology may be observed in the 3rd-5th day, characterised by pelvic-abdominal pain associated with peritoneal reaction, nausea and fever.
This symptomatology persists for a few days and resembles a spontaneous complication of fibroids: aseptic necrosis.
Generally, for fibroids less than 8 cm in diameter, discharge occurs the day after surgery.
The patient will be checked within 2 months after an echo-colour Doppler is performed.
The efficacy of the treatment is evaluated with: anamnesis and objective examination, to check the evolution of the haemorrhagic and compressive symptoms; haemochrome, to monitor anaemia, and CPK to check the correlation between the fall in CPK rates and the reduction in fibroid volume; colour-echo-Doppler to follow the reduction in fibroid volume and the disappearance of the peritumoral vascular network.
The patient will be reviewed by the gynaecologist with the same examinations at 6 months, at 12 months and then annually.
The effectiveness on menometrorrhagia is immediate, while to appreciate the volumetric reduction of the uterine fibroid one has to wait 4-6 months: the process starts no earlier than 4 weeks and continues for 8-12 months especially for large fibroids.
Results
The French multicentre study, conducted on 200 women aged 34-49 years with one or more symptomatic fibroids and with a follow-up of 6 to 60 months on 186 women, yielded the following results
- technical impossibility of catheterising the uterine arteries in 7% of cases (different operators);
- disappearance of menometrorrhagia in 92% of cases;
- reduction in fibroid volume of more than 70% in two thirds of cases, and reduction of more than 40% in one third of cases;
- 8 failures, which required traditional surgery; no relapse of fibromatosis was recorded;
- 7 unwanted pregnancies were recorded, 3 aborted for private reasons and 4 carried to term normally.
Complications included 12 amenorrhoeas, 7 of which were transient and 5 definitive (women over 45 years of age).
In addition, only one serious complication was observed for a voluminous pedunculated subserous fibroid that led to a hysterectomy with partial colectomy.
In our Brescian case series, 62 women with symptomatic uterine fibroids were treated by embolisation at the end of 1998.
No technical impossibility of catheterisation (single operator) and no intraoperative complications were observed during the operation.
The patients were discharged within 48/72 hours. The follow-up of more than 6 months in 29 women gave the following results:
- return to normal for the symptom menometrorrhagia in all women;
- reduction of fibroid volume by more than 70% in 89% of the cases, and reduction between 40 and 60% in 10% of the cases (these were large, old uterine fibroids).
Complications included 3 cases of amenorrhoea, one of which was definitive in a 48-year-old woman.
To date, the number of patients treated with embolisation is more than 200, with results overlapping with the first series.
Conclusions
According to the works in the literature and our experience, we can state that:
- arterial embolisation with microparticles represents a real alternative to invasive surgery;
- compared with hormone therapy, embolisation avoids lengthy protocols with major side effects;
- the psychological and sexual consequences are nil and pregnancies possible;
- according to various studies, this technique could eliminate 90% of hysterectomies and 70% of conservative operations for uterine fibroids.
Currently, the indications for embolisation are also aimed at younger women; in fact, the more recent the fibroid, the better it responds to the operation (with total disappearances of fibroids of less than 6 cm).
The results for cases of multiple fibroids, even recurrent ones, are good and embolisation has the specificity of treating all fibroids at the same time, even invisible ones in the process of formation.
A worldwide survey of about 2000 women undergoing embolisation indicates a satisfaction rate of over 90%.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
The Use Of Outpatient Hysteroscopy For Early Diagnosis
Utero-Vaginal Prolapse: What Is The Indicated Treatment?
Pelvic Floor Dysfunction: What It Is And How To Treat It
Pelvic Floor Dysfunction: Risk Factors
Salpingitis: Causes And Complications Of This Fallopian Tube Inflammation
Hysterosalpingography: Preparation And Usefulness Of The Examination
Endometriosis: Symptoms, Diagnosis And Treatment
Pap Test, Or Pap Smear: What It Is And When To Do It
Urinary Tract Infections: Symptoms And Diagnosis Of Cystitis
Vulvodynia: What Are The Symptoms And How To Treat It
What Is Vulvodynia? Symptoms, Diagnosis And Treatment: Talk To The Expert
Total And Operative Hysterectomy: What They Are, What They Involve
Pap Test, Or Pap Smear: What It Is And When To Do It
Drugs Used In Obstetric Emergencies To Modify Uterine Contractions


