What is an implantable defibrillator (ICD)?
An implantable defibrillator is a cardiac pacemaker powered by a battery, which monitors the heart’s electrical signals and delivers an electric shock when it detects an abnormal rhythm of a certain type
The pacemaker is about the size of a small bar of soap.
Why is a defibrillator implanted?
Sometimes abnormal, extremely rapid heart rhythms occur, which are called tachyarrhythmias.
The electrical signals may originate from the ventricles instead of the natural pacemaker, the SA node, resulting in a type of arrhythmia called ventricular tachycardia (VT), which can cause a strong acceleration of the heartbeat.
QUALITY AED? VISIT THE ZOLL BOOTH AT EMERGENCY EXPO
Cardiac acceleration leads to a reduction in the cardiac pumping capacity, as the heart muscle does not have enough time to fill up with blood; if this condition persists, oxygenation deficits can occur in the brain and fainting, dizziness, altered vision up to loss of consciousness and cardiac arrest can occur.
Another type of arrhythmia is ventricular fibrillation (VF), which can originate at different points in the ventricles. In this case, the heartbeat is extremely accelerated, up to 300 b/min, and cardiac contractions are no longer effective (the heart chambers instead of contracting ‘vibrate’); this condition leads to cardiac arrest.
Both VT causing loss of consciousness and VF if not stopped in a very short time result in irreversible damage to brain tissue and death.
Ventricular tachyarrhythmias can occur in individuals of all ages.
They occur most frequently in heart patients, but can also occur in apparently healthy individuals.
Sometimes VT can develop into VF.
Sudden death due to cardiac arrest affects about 1 person per 1000 inhabitants per year.
Medications or surgical procedures can be used to prevent or interrupt tachyarrhythmias.
In many cases, the implantable defibrillator (ICD) can be used
The defibrillator delivers electrical energy to the heart to slow down or interrupt the arrhythmia and restore a normal rhythm.
ICDs are usually implanted to treat heart arrhythmias that are too fast, but most systems can also treat slow rhythms (bradycardias).
Many people suffer from dangerous arrhythmias.
It is not always easy to arrive at a diagnosis of ventricular arrhythmias.
An electrocardiogram can be used initially, but further tests are usually necessary to determine the cause or possible treatment of VT or VF.
Electrophysiological study, the recording of endocavitary cardiac electrical activity carried out in the hospital by an electrophysiologist who places catheters at the level of the heart through which normal cardiac electrical signals and the reaction to induced impulses are recorded, can be extremely useful.
How does an implantable defibrillator work?
An ICD can use one or more types of energy to help the heart resume a normal rhythm:
- Antitachycardia pacing (ATP): if the rhythm is regular but accelerated, the ICD system can deliver a series of small, rapid electrical impulses used to interrupt the arrhythmia and restore a normal rhythm;
- Cardioversion: if the arrhythmia is regular but very rapid, the ICD can deliver a low-energy discharge that can interrupt the arrhythmia;
- Defibrillation: for extremely rapid and irregular arrhythmias, high-energy discharges can interrupt the arrhythmia and restore a normal rhythm.
What does an implantable defibrillator look like?
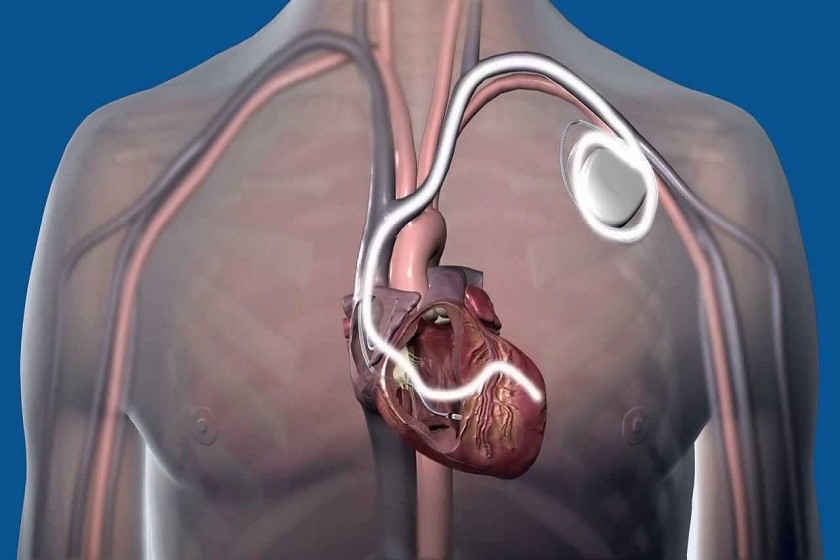
All ICDs comprise a pacemaker that generates the energy to interrupt tachyarrhythmias and the lead(s) that deliver the energy to the heart.
The leads themselves transmit signals from the heart to the device, so the pacemaker is able to monitor cardiac activity and respond with appropriate therapy.
One end of the lead is connected to the pacemaker, the other is placed in a cardiac chamber.
Another component of the ICD system is the monitoring device used by medical personnel.
After implantation, the ICD functions must be checked and adjusted if necessary.
The memory of the pacemaker stores information on cardiac activity before, during and after an arrhythmia and stores the treatment delivered.
How is the defibrillator implanted?
The procedure for implanting the ICD is very similar to that for implanting a normal pacemaker.
Here too, the procedure is conducted under local anaesthesia, and the system is generally implanted under the collarbone.
In most cases, the leads are placed by passing them through a vein into the heart chamber.
During the operation, the entire ICD system is tested by inducing the arrhythmia so that the system detects it and delivers the programmed treatment.
After implantation
After the operation, the hospital stay is short; before discharge, the ICD may be tested again.
The system delivers treatment based on what it registers.
Several sensations have been described during energy delivery.
Antitachycardia stimulation: it is possible not to feel the delivered discharge or to feel a sensation of stimulation in the chest.
Patients claim it is painless;
Cardioversion: these low-energy discharges are stronger than the stimulation pulses. Several patients claim they feel a slight discomfort, such as a jolt to the chest;
Defibrillation: the discharge may be felt as a ‘kick to the chest’ and may be preceded by a subjective sensation of tachycardia or fainting;
Stimulation by bradycardia: this is not usually perceived by patients.
Normally, people can gradually return to their usual activities.
Restrictions are sometimes applied; a few seconds of unconsciousness during activities such as driving could be dangerous for oneself and others.
It is up to the doctor to discuss any restrictions with the patient.
Before being discharged from hospital, the patient receives an identity card, which he/she must carry with him/her at all times.
You may also be given an ICD safety card that explains how the implanted system can set off alarms at security checkpoints.
It is extremely important to attend regularly scheduled check-ups to ensure that the device is functioning properly and that the battery charge remains.
When the battery is close to exhaustion, the stimulator is scheduled to be replaced.
The general rule for ICD patients is to keep away from devices that generate high interference such as large electrical generators.
- Maintain a distance of at least 30 cm between the ICD and the following sources
- loudspeakers of large stereo equipment
- powerful magnets;
- magnetic wands used by airport security;
- portable battery-powered tools;
The vast majority of electrical appliances with which one normally comes into contact pose no problem.
Most electrical appliances and devices such as PCs, fax machines, printers are safe and do not affect the operation of the ICD.
An ICD may only be sensitive to anti-theft or security systems if the wearer lingers nearby.
Airport security alarms use magnetic fields, so it is important to carry the ICD with you at all times.
For mobile phones: maintain a distance of at least 15 cm between the mobile phone and the ICD, keep the device on the opposite side of the body to the stimulator.
Follow special precautions for the following procedures:
- diathermy (skin heating with instruments that produce short waves or microwaves);
- electrocautery: should be used with the ICD system switched off;
- nuclear magnetic resonance, the magnets could damage the device.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
What Is The Difference Between Pacemaker And Subcutaneous Defibrillator?
Heart Disease: What Is Cardiomyopathy?
Inflammations Of The Heart: Myocarditis, Infective Endocarditis And Pericarditis
Heart Murmurs: What It Is And When To Be Concerned
Broken Heart Syndrome Is On The Rise: We Know Takotsubo Cardiomyopathy
Cardiomyopathies: What They Are And What Are The Treatments
Alcoholic And Arrhythmogenic Right Ventricular Cardiomyopathy
Difference Between Spontaneous, Electrical And Pharmacological Cardioversion
What Is Takotsubo Cardiomyopathy (Broken Heart Syndrome)?
Dilated Cardiomyopathy: What It Is, What Causes It And How It Is Treated
Heart Pacemaker: How Does It Work?
World Heart Day 2022: Moves For A Healthy Heart
Heart Disease Facts And Statistics: What You Need To Know


