When is a colonoscopy with biopsy necessary?
Colonoscopy is a diagnostic test performed to visualise the inside of the colon and rectum, which is carried out in order to investigate the causes of any abnormal intestinal symptoms complained of by the patient
The test consists of inspecting the final tract of the digestive tract with a probe that is introduced anally and is equipped with a mini-video camera at its apex.
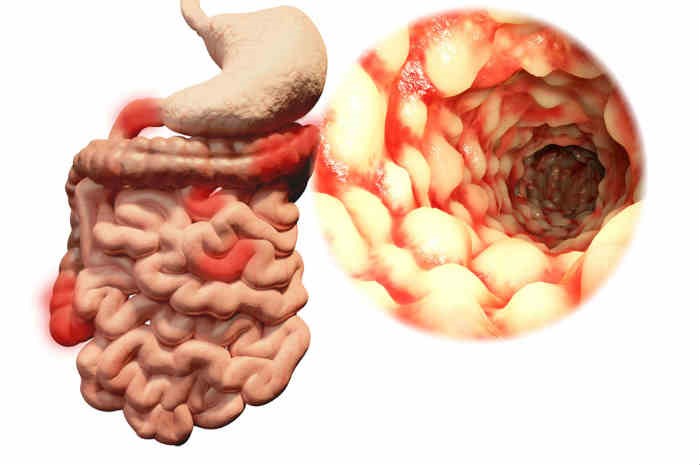
The images transmitted from the instrument (colonoscope) to the special screen allow the doctor to assess the health of the colon, detecting the possible presence of ulcers and inflamed tissue, abnormal cell growth, benign and malignant tumours.
WHAT IS COLONOSCOPY USED FOR?
Colonoscopy is a visual test that allows the doctor performing it to have an immediate view of any morphological changes in the mucous membrane of the colon and to detect possible abnormal formations such as polyps and tumours, thus being able to make a rapid diagnosis.
Usually, colonoscopy is performed if there is a family history of intestinal disease, or, from the age of 50, as a prevention against colorectal cancer, to look for any early signs of cancer.
COLONOSCOPY WITH BIOPSIES AND INTERVENTIONS
In addition to exclusively diagnostic purposes, colonoscopy can also be used to perform biopsies and therapeutic interventions.
In fact, colonoscopy allows for the simultaneous cleaning of the walls of the colon, aspiration of intestinal contents, taking of samples and actual surgery.
HOW AND WHERE DOES IT TAKE PLACE?
Colonoscopy is performed on an outpatient basis.
Shortly before the start of the test, the doctor may administer painkillers, sedatives and muscle relaxants to promote muscle relaxation and relieve any discomfort the patient may be experiencing.
Next, the patient lies on his or her left side and the doctor proceeds to insert the colonoscope, a small flexible probe equipped with a mini-video camera and a light source, into the anus, which is moved up along the various intestinal tracts until it reaches the cecum.
In order to obtain better distension of the intestinal walls, so as to facilitate visualisation of the mucosa, the doctor proceeds to insufflate carbon dioxide through the colonoscope.
HOW LONG DOES A COLONOSCOPY LAST?
A colonoscopy lasts approximately 30 to 60 minutes.
PREPARATION RULES
A colonoscopy requires preparation that begins a few days before it is actually performed. In particular, in the three days preceding the test, the patient must follow a low-fibre diet, avoiding eating fruit, vegetables and whole-grain cereals, as well as drinking alcohol and fruit juices.
On the day immediately preceding the colonoscopy, the patient should follow an exclusively liquid diet in order to promote the elimination of faeces and the consequent clearing of the intestinal tract to be examined.
Also for this purpose, the patient will be advised to use a laxative and/or to take an enema.
During the preparation phase, the patient may continue to take his or her usual medication and/or supplements, but taking care to discuss this with the doctor who will be performing the colonoscopy to assess possible interactions.
PRECAUTIONS AFTER THE TEST
At the end of the test, the patient may be advised to rest for 30 to 120 minutes to give the sedatives used time to wear off.
Since the drugs used may cause drowsiness and exhaustion, it is advisable for the patient to be accompanied to the test and to rest for the rest of the day afterwards.
In the hours immediately following the conclusion of the colonoscopy, the patient may experience cramping and abdominal bloating due to the air insufflated during the test.
These are common phenomena that should not cause alarm as they resolve spontaneously and in a short time.
After the colonoscopy, the patient can resume eating, preferring light and easily digestible foods.
If the patient underwent a biopsy or polypectomy (removal of polyps) at the same time as the colonoscopy, a slight bleeding from the anus may occur during the first defecation after the test.
This is normal and should not cause concern.
On the other hand, if bleeding persists, it is advisable to seek medical advice immediately.
The same applies if abdominal pain or high fever occurs in the days following the colonoscopy.
ANY CONTRAINDICATIONS OR RISKS
Colonoscopy is a low-risk diagnostic procedure. The incidence of serious complications is very rare and is mainly related to polypectomy.
Complications caused by the sedatives used during the test may rarely occur, against which, however, antagonistic substances of proven effectiveness are available.
Colonoscopy is not recommended in cases of acute diverticulitis, toxic megacolon and in the recovery phase following surgery performed in this same section of the intestine.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Colonoscopy: What It Is, When To Do It, Preparation And Risks
Colon Wash: What It Is, What It Is For And When It Needs To Be Done
Rectosigmoidoscopy And Colonoscopy: What They Are And When They Are Performed
Ulcerative Colitis: What Are The Typical Symptoms Of The Intestinal Disease?
Wales’ Bowel Surgery Death Rate ‘Higher Than Expected’
Irritable Bowel Syndrome (IBS): A Benign Condition To Keep Under Control
Intestinal Infections: How Is Dientamoeba Fragilis Infection Contracted?
Study Finds Link Between Colon Cancer And Antibiotic Use
Colonoscopy: More Effective And Sustainable With Artificial Intelligence
Colorectal Resection: In Which Cases The Removal Of A Colon Tract Is Necessary
Gastroscopy: What The Examination Is For And How It Is Performed
Gastro-Oesophageal Reflux: Symptoms, Diagnosis And Treatment
Endoscopic Polypectomy: What It Is, When It Is Performed
Straight Leg Raise: The New Manoeuvre To Diagnose Gastro-Oesophageal Reflux Disease
Gastroenterology: Endoscopic Treatment For Gastro-Oesophageal Reflux
Oesophagitis: Symptoms, Diagnosis And Treatment
Gastro-Oesophageal Reflux: Causes And Remedies
Gastroscopy: What It Is And What It Is For
Colonic Diverticular Disease: Diagnosis And Treatment Of Colonic Diverticulosis
Gastro-Oesophageal Reflux Disease (GERD): Symptoms, Diagnosis And Treatment
Diverticula: What Are The Symptoms Of Diverticulitis And How To Treat It
Irritable Bowel Syndrome (IBS): A Benign Condition To Keep Under Control
Gastroesophageal Reflux: Causes, Symptoms, Tests For Diagnosis And Treatment
Non-Hodgkin’s Lymphoma: Symptoms, Diagnosis And Treatment Of A Heterogeneous Group Of Tumours
Helicobacter Pylori: How To Recognise And Treat It
A Baby’s Gut Bacteria May Predict Future Obesity
Sant’Orsola In Bologna (Italy) Opens A New Medical Frontier With Microbiota Transplantation
Microbiota, The Role Of The ‘Gate’ That Protects The Brain From Intestinal Inflammation Discovered
What Are The Differences Between Diverticulitis And Diverticulosis?


