Pulmonary ventilation: what a pulmonary, or mechanical ventilator is and how it works
Pulmonary ventilation is not just a procedure that the patient needs: this year’s Covid-19 has also made it the epitome of how and how much healthcare intervention by the rescuer has changed
Exactly one year ago, a large proportion of ambulance transports involved trauma patients, as well as intra- and extra-hospital transports.
Today, pulmonary ventilation plays a role, and it is essential to be familiar with it, even if only in brief.
Yes, what is pulmonary ventilation? What role does the lung ventilator play in the daily life of a rescuer or healthcare worker?
Pulmonary, artificial or mechanical ventilation replaces or supports the inspiratory muscles’ activity, ensuring an adequate gas volume to the lungs.
It is a mechanical, automatic and rhythmic process, regulated by the higher centres through which, by the skeletal muscles of the diaphragm contraction and relaxation, abdomen and rib cage, is promoted the exchange of air in the alveoli.
During inhalation, the intra-alveolar pressure becomes slightly negative compared to atmospheric pressure (-1mmHg), and this causes air to flow inwards along the airways.
On the other hand, during normal exhalation the intra-alveolar pressure rises to around +1mmHg, causing air to flow outwards.
The device that performs this task is called a lung ventilator or mechanical ventilator or artificial ventilator.
The lung ventilator replaces the respiratory system mechanical functions in whole or in part when the respiratory system becomes incapable of performing its task on its own due to disease, trauma, congenital defects or medication (e.g. anaesthetics during surgery).
The ventilator can insufflate a kind of gas mixture into the lungs allowing them to exhale with known frequency and appropriate pressure.
In order to deliver the necessary amount of oxygen to the patient and remove the carbon dioxide produced, the ventilator must be able to:
– insufflate controlled amounts of air or gas mixtures into the lungs;
– stop insufflation;
– allow the exhaled gases to escape;
– repeat the operation continuously.
In contrast to natural ventilation, in artificial ventilation by means of a lung ventilator, the pressure is positive not only in the upper airways but also intrathoracically.
In order to expand the lungs and the rib cage, the ventilator must send air at pressure: the lungs are always at atmospheric pressure, even when there is no flow.
Mechanical ventilation, being at positive pressure, leads to an increase in respiratory exchanges, with the reopening of poorly ventilated areas to ventilation, but can at the same time lead to injury to the respiratory system (barotrauma).
Mechanical ventilation is used in cases of:
– acute severe lung disease
– apnoea associated with respiratory arrest (also from intoxication);
– severe and acute asthma;
– acute or chronic respiratory acidosis;
– moderate/severe hypoxemia;
– excessive respiratory work;
– paralysis of the diaphragm due to Guillain-Barré syndrome, Myasthenia Gravis, acute crises of muscular dystrophy or amyotrophic lateral sclerosis, spinal cord injury, or the effect of anaesthetics or muscle relaxants;
– increased work of the respiratory muscles, evidenced by excessive tachypnoea, supraclavicular and intercostal re-entry and large movements of the abdominal wall;
– hypotension and shock, as in congestive heart failure or sepsis.
Pulmonary ventilation, types of lung ventilators
There are different types of mechanical ventilators:
– negative pressure mechanical ventilator
– positive pressure mechanical ventilator
– mechanical intensive care or sub-intensive care ventilator (or emergency/medical emergency transport)
– mechanical ventilator for non-natal intensive care or sub-intensive care (or emergency/medical emergency transport)
In addition, mechanical ventilators are divided into:
– Invasive Ventilation
– Non-Invasive Ventilation
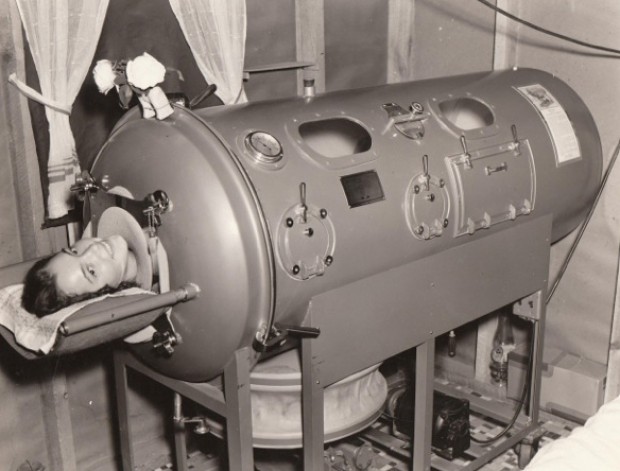
Negative pressure mechanical/artificial ventilator
Negative pressure mechanical ventilation represents the first generation of mechanical lung ventilators, also known as steel lungs.
The steel lung, in a nutshell, merely reproduces the mechanic respiratory recorded on normal conditions which myopathy or neuropathy makes it impossible by an insufficient function of the rib cage muscles.
Negative pressure systems are still in use, mostly on patients with thoracic insufficient cage muscles, as in poliomyelitis.
Positive pressure mechanical/artificial ventilator (non-invasive)
These instruments are designed for non-invasive ventilation, including at home for the treatment of obstructive sleep apnoea.
The ventilator works by insufflating gas mixtures (usually air and oxygen) at positive pressure into the patient’s airways.
Home ventilators (electromechanical power source)
Piston or reciprocating pump: Collects gases even at low pressure, mixes them and pushes them into the external circuit during the inspiratory phase.
Less effective in compensating for leaks
Turbine: Draws in gases, compresses them and sends them to the patient via a one-way inspiratory valve.
They can control pressure by flow and volume delivery.
Home ventilators (turbine with low-pressure gas supply system):
1. CPAP and autoCPAP
- Bi-level
3. Pressovolumetric
1. CPAP and autoCPAP (not ventilation mode but the type of ventilator)
– are used for the treatment of sleep disorders;
– CPAP provides a predetermined level of equal positive pressure in both phases of breathing that prevents airway collapse;
– self CPAP delivers positive pressure in both phases of breathing according to the patient’s needs at that particular time (a pressure range is set).
2. Bi-level
– non-invasive ventilation machine offering two pressure levels: IPAP (positive pressure in the inspiratory phase) and EPAP (positive pressure in the expiratory phase);
– do not allow monitoring of ventilatory parameters;
– they are used for the treatment of sleep disorders;
– when CPAP does not correct apnoea and/or for severe apnoea or associated hypoxemia.
3. Pressuvolumetric ventilators
These allow the use of pressurized or volumetric modes of ventilation. They are distinguished by the circuit used.
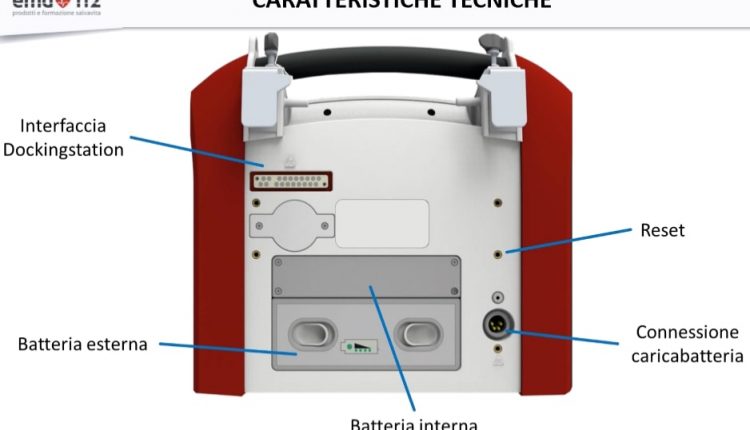
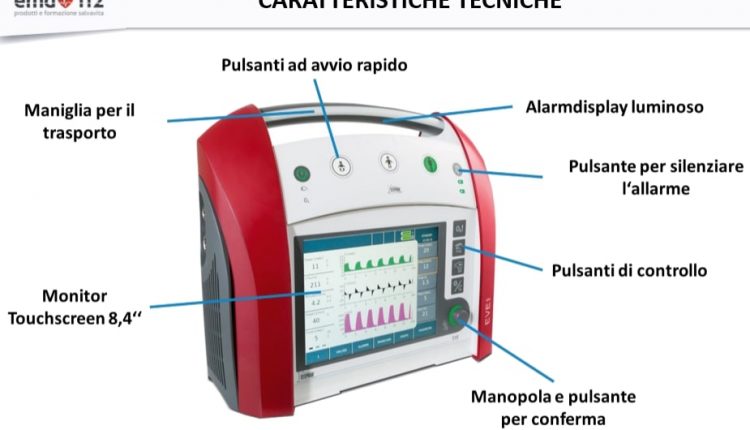
Pulmonary ventilation in intensive care (pneumatic energy source)
 Lung ventilators can operate in both invasive and non-invasive modes of ventilation, few of the main features are:
Lung ventilators can operate in both invasive and non-invasive modes of ventilation, few of the main features are:
– They work with high-pressure compressed gas (4 BAR)
– Provide FiO2 stability
– They guarantee volume delivery even in case of high impedance (obese patient)
FiO2 is the inhaled fraction of O2. It is an acronym used in medicine to indicate the % of oxygen (O2) inhaled by a patient.
FiO2 is expressed as a number between 0 and 1 or as a percentage. The FiO2 in atmospheric air is 0.21 (21%).
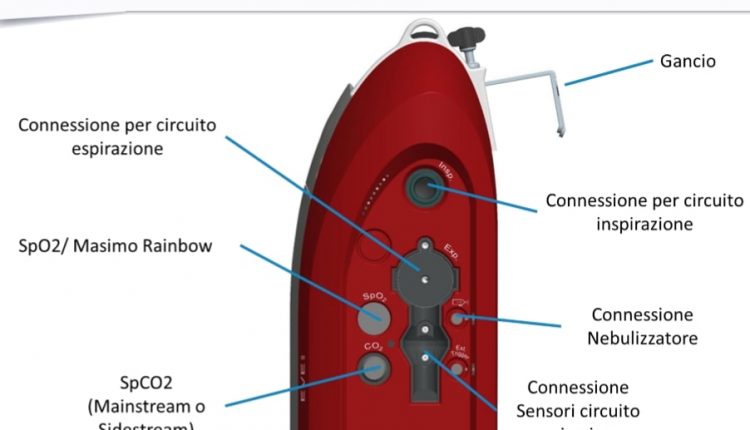
The lung ventilator consists of the following basic functional blocks
– a positive pressure generator able to produce a pressure gradient between the external atmospheric pressure environment and the alveoli, determining the amount of gas flow to be insufflated to the patient.
This function is achieved either by generating a force that is applied to a bellows containing the insufflating gas mixture, or by reducing the gases pressure of the fixed system through a series of cascade valves;
– a metering system for the current volume (VT);
– a series of respiratory cycle timing devices which, by appropriately opening and closing the valves controlling the inspiratory and expiratory flows, allow the transition from inspiration to expiration and vice versa;
– a patient circuit, comprising all the parts that connect the ventilator with the patient’s respiratory system. There can be open circuits (without re-breathing), which at each exhalation discharge the exhaled gases to the outside, or closed circuits with CO2 absorbers by means which the patient’s exhaled gas is recovered after the CO2 absorption;
– resistive elements comprising all the ducts interposed between the positive pressure generator and the patient’s respiratory system that produce a resistance to the advancement of gas into them.
Pulmonary ventilation: how a ventilator works
Lung ventilators offer different modes of operation to be adapted according to the specific needs of the patient.
The fundamental criterion on which medical personnel base their choice of ventilation model is the patient’s ability to breathe independently.
The controlled mode is chosen when the patient has no spontaneous respiratory activity and requires the physician to adjust the operating times (inspiration duration, expiration duration, pause duration, inspiratory frequency) on the lung ventilator control panel.
There are two possibilities for controlled ventilation: constant flow ventilation and constant pressure ventilation, depending on the chosen quantity (flow or pressure) as the ventilation system control parameter.
The assisted mode is used for difficulty breathing patients still able to start the inspiratory phase.
The lung ventilator must be aware of the patient’s attempt to inspire and assist in doing so.
Finally, the synchronized mode consists of an initial phase in which the patient is ventilated by sending a certain volume of air into the lungs in a predefined interval time, in a controlled constant-flow mode; this is followed by spontaneous respiration period if the patient has recovered his respiratory system functionality, or by an assisted ventilation period in case of persistent difficulty.
Read also:
Manual Ventilation, 5 Things To Keep In Mind
COVID-19 Patients: Does Inhaled Nitric Oxide During Mechanical Ventilation Give Benefits?
FDA Approves Recarbio To Treat Hospital-Acquired And Ventilator-Associated Bacterial Pneumonia
Source:
Ventilatore Polmonare Stephan ® EVE IN per terapia intensiva e trasporto intra-ospedaliero