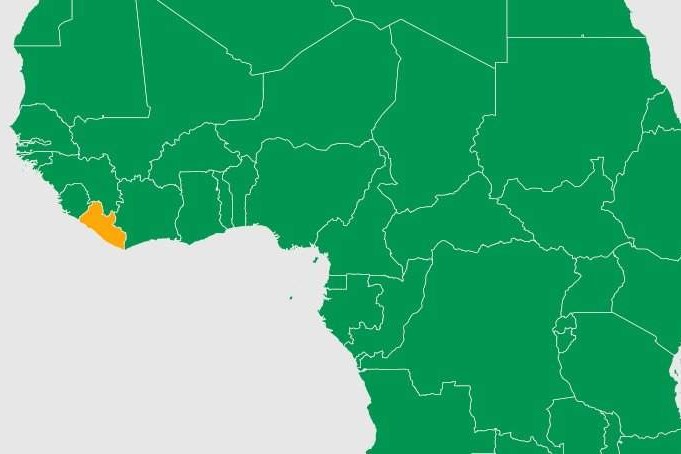
Africa, WHO engaged in antimicrobial resistance protection in Liberia
The threat of AMR (antimicrobial resistance) and prescribing without justification: antimicrobial is the collective term for antibiotics, antivirals, antifungals and pesticides
Antimicrobial resistance, or AMR, occurs when bacteria, fungi, parasites and viruses that make humans and animals sick become resistant to drugs designed to kill these invaders.
AMR (antimicrobial resistance) is a major public health crisis across Africa
The WHO estimates that AMR could kill 4.1 million people in Africa by 2050 unless more prudent drug-taking practices are followed by medical facilities and individuals (who, for example, do not follow the full course of drugs or take them when they are not needed).
In the evaluation of Phoebe Hospital, a hospital in the capital city of Bong (Liberia), data collected from medical records using the WHO point prevalence survey indicated that the majority (517, or 63%) of patients put on antibiotics had no laboratory results confirming the presence of an infection.
Liberia developed a national action plan on antimicrobial resistance in 2018
Its practices became more rigorous, however, with national guidelines on antimicrobial stewardship followed in 2021, with support from WHO and other partners to improve surveillance and promote the rational use of antimicrobial drugs in health facilities.
The support included ICT equipment to strengthen surveillance and conduct a baseline assessment of antibiotic prescribing and resistance in the seven hospitals.
In addition, 36 frontline health workers were trained on antimicrobial susceptibility testing, with a focus on diagnostic stewardship.
78 frontline health workers at national and facility levels received technical training on effective antimicrobial stewardship to become members of the medical quality management teams established in each of the seven hospitals.
Across Africa, WHO is working with ministries of health and health institutions to instil sound antimicrobial stewardship
Where it is practised, stewardship appears to improve demand for laboratory services from doctors and patients.
Medical quality management teams in Liberia, for example, meet regularly to plan, implement and monitor interventions on the prescription and use of essential drugs, with a focus on antibiotics and antimalarials.
Ward rounds and clinical conferences are routinely organised to discuss patient conditions and their treatment using hospital-specific action points, ultimately improving antimicrobial stewardship interventions.
“We have seen gradual improvements in antimicrobial susceptibility testing and reporting between 2021 and 2022, compared to the past,” reports William Walker, laboratory technician and microbiologist at Phebe Hospital.
“If the hospital’s diagnostic infrastructure and staff technical capacity are further strengthened, it will go a long way to promote early detection and reporting of AMR pathogens and better monitoring of antimicrobial prescribing and use.”
According to the senior pharmacist at Liberia’s Redemption Hospital, Dr Munyah Mohamed Karvah, the pharmacy no longer accepts open orders from doctors or clinicians who do not have laboratory tests.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
The Use Of Antibiotics According To The New WHO Guidelines
Antibiotics Resistant Bacteria: The Important Discovery Of Australia
Bacterial Infections: When To Use Antibiotics?
The Lancet: Antibiotic Resistance Kills Millions Worldwide
Cystitis, Antibiotics Are Not Always Necessary: We Discover Non-Antibiotic Prophylaxis
Oxygen-Ozone Therapy To Combat Antibiotic Resistance
Africa, Tuberculosis & HIV In Pregnancy: A Concerning State Of Affairs
Pregnant Women: Addressing Maternal Mental Health In Africa


