Colour changes in the urine: when to consult a doctor
It may happen that our urine has a different appearance than usual. In certain conditions, it is advisable to seek medical advice and undergo diagnostic tests to investigate the problem
But what are the changes we can recognise in the colour of our urine and when should we be concerned?
Clear, yellow urine
Throughout history, diseases of the urinary system (kidneys, ureters, bladder and urethra) have been diagnosed by changes in the colour of urine.
Today, although a variety of diagnostic tools are available, analysis of the colour and appearance of urine is still essential in the process of diagnosing possible diseases of the urinary system, i.e. the kidneys, ureters, bladder and urethra.
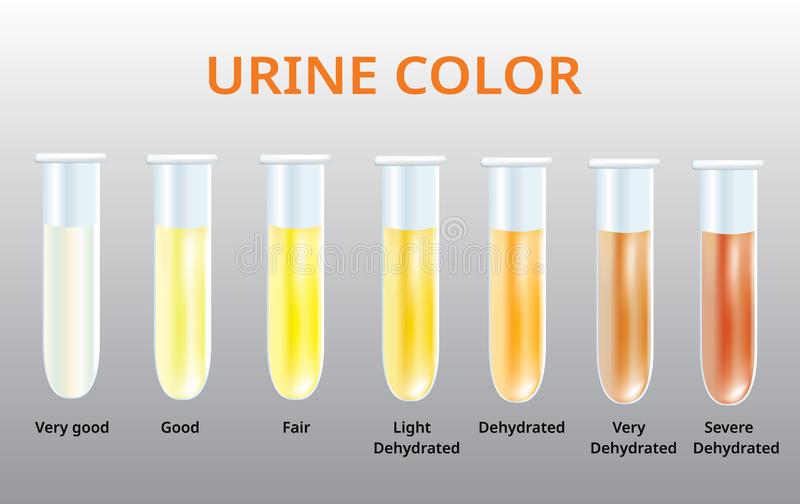
Under normal conditions, urine has a more or less marked yellow colour and a clear appearance.
The different colours may be due to the presence of kidney, urological or systemic diseases, and the various degrees of turbidity are related to suspended corpuscles.
However, changes in urine colour and clarity are not necessarily associated with problems.
Dark-coloured and strong-smelling urine
Darker-than-normal and stronger-smelling urine, for example, can also indicate dehydration, or particularly heavy sweating.
As the lost fluids are replenished, the urine will return to its usual colour.
Taking certain medications can also lead to dark urine, as pigmentation of the urine is part of the unwanted effects of these medications.
If, on the other hand, the dark colour is associated with a cloudy, foul-smelling appearance and pain on urination, an infection may be the cause.
In more severe cases, dark urine may be associated with an excess of bilirubin from the liver or other substances such as muscle enzymes, or it may be related to malfunctioning parts of the urinary system.
Red-coloured urine and blood in the urine
Reddish-coloured urine may indicate haematuria, i.e. blood in the urine.
If the blood is distinguishable by the colour of the urine, it is called macrohaematuria. If it is not visible to the naked eye and is detected by physical-chemical urine analysis, it is called microhaematuria.
Blood in the urine can have several causes.
For example, exertional haematuria implies the presence of reddish-coloured urine after very intense physical training and occurs mainly after running.
Hematuria can also be caused by pelvic trauma, for example from contact sports.
However, blood in the urine can come from any organ in the urinary tract and can occur in isolation or in association with other symptoms, such as abdominal pain or difficult urination.
Foam in the urine
Foam in the urine does not necessarily mean that there is anything wrong with the urine.
Foaming can be caused by particularly fast urine output, dehydration or even detergent residues in the toilet.
Foam in the urine is also associated with treatment with certain medications and urinary tract infections.
If the problem continues or worsens, it may indicate proteinuria, which is an abnormal presence of protein in the urine.
Which urine tests should be done in case of colour changes?
In case of dark coloured urine, haematuria or foam in the urine, without these phenomena being associated with physical exertion, dehydration or the intake of new medicines, it is a good idea to contact your general practitioner who, if necessary, will indicate the appropriate tests to be carried out: usually urine chemistry and urine culture, which are essential to identify the possible causes.
Urinalysis is a simple, non-invasive test that can be used to diagnose kidney and urological disorders at an early stage, and should therefore be included in every routine check-up.
If the urine chemistry indicates that something is amiss, a nephrology/urology specialist should be consulted and further investigations such as microscopic urine sediment analysis, ultrasound of the urinary tract and specific blood tests should be performed. In more severe situations, second-level tests (uro-CT or uroRMN) or renal biopsy may be necessary.
Each laboratory alteration must always be placed in the clinical context of the individual.
Read Also:
Pediatrics: Serious Cases Of Type 1 Diabetes In Liguria Doubled Since The Start Of Covid Pandemic
Pan-Resistance, Candida Auris In US Hospitals: Warning From CDC Atlanta